(UroToday.com) The 2024 American Society of Clinical Oncology (ASCO) Annual Meeting held in Chicago, IL between May 31st and June 4th, 2024 was host to a prostate, testicular, and penile cancers poster session. Dr. Zachary Klaassen presented an analysis of the impact of mental health illness prior to prostate cancer diagnosis on subsequent treatment received and prostate cancer outcomes.
Men with mental health illnesses are 20% less likely to be diagnosed with prostate cancer. However, when diagnosed, they have a two-fold increased odds of harboring aggressive prostate cancer, compared to men without mental health illnesses. It remains unknown whether prostate cancer patients with mental health illnesses have comparable treatment rates and post-treatment outcomes, compared to prostate cancer patients without mental health illnesses. The objective of this study was to compare definitive treatment rates, adherence to surveillance following definitive therapy, and biochemical recurrence rates between prostate cancer patients with and without mental health illnesses.
This was a national, retrospective study that used a matched cohort of male veterans who were diagnosed with prostate cancer following a recent mental health illness diagnosis (i.e., within the preceding three years) or diagnosed with prostate cancer in the absence of a mental health illness between 2000 and 2020. Men were inclusion-eligible if they were:
- Active users of the Veterans Affairs (VA) system, defined as ≥2 encounters with a VA provider within a five-year period between 2000 and 2020
- Age at diagnosis was between 40 and 80 years
- Had no prior malignancy
Competing risk analysis with cumulative incidence estimates were used to estimate the association between the presence of a mental health illness and time from prostate cancer diagnosis to receipt of definitive therapy (radical prostatectomy or radiotherapy). The competing risk in this model was any-cause death. The association between presence of a mental health illness and adherence to surveillance, defined as ≥3 PSAs within the first year following definitive therapy and ≥1 PSA during each following year for four consecutive years, was evaluated using logistic regression modeling. The association between the presence of a mental health illness and time from definitive therapy to biochemical recurrence (AUA and Phoenix criteria for biochemical failure post-radical prostatectomy and radiotherapy, respectively) was evaluated using competing risk modeling.
This study included 52,407 men diagnosed with prostate cancer, of whom 19,976 had a mental health illness diagnosis. The cumulative incidence of definitive therapy was higher for those with a mental health illness (36% vs. 27% after 10 years). Men with pre-existing MHI were significantly more likely to receive definitive therapy for prostate cancer, compared to men without mental health illness (multivariable analysis: HR= 1.34, 95% CI= 1.30–1.39).

Among men treated for prostate cancer (n=15,972), adherence to surveillance was similar for those with or without a mental health illness (proportions: 45% and 46%, respectively). The odds of adhering to surveillance did not differ significantly between the subgroups on univariable analysis (OR= 0.96, 95% CI= 0.89-1.04); however, on multivariable analysis, the odds of surveillance adherence were lower in those with a mental health illness (OR= 0.92, 95% CI= 0.85–1.00, p=0.049).
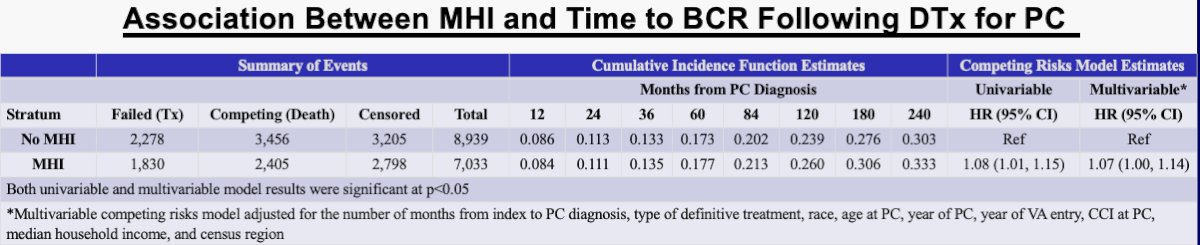
The cumulative incidence of biochemical recurrence following definitive therapy was higher in men with a mental health illness (31% versus 28% after 15 years). The rate of biochemical recurrence was significantly higher for such men on both univariable (HR= 1.08, 95% CI= 1.01– 1.15) and multivariable analyses (HR= 1.07, 95% CI= 1.00–1.14).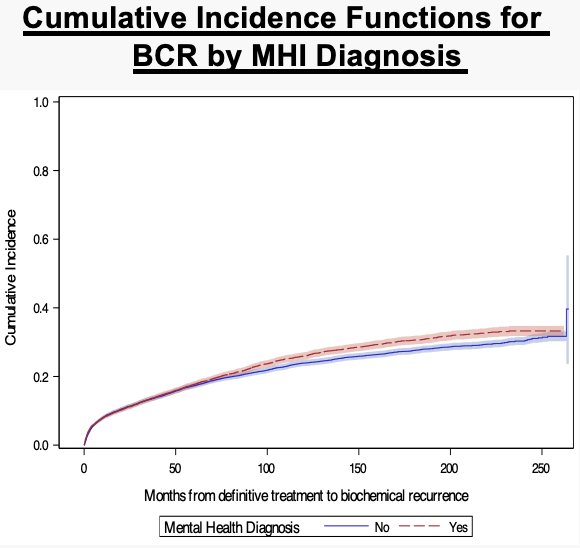
Dr. Klaassen concluded that:
- Men with a mental health illness prior to a prostate cancer diagnosis are more likely to receive definitive therapy compared to prostate cancer patients without a mental health illness.
- Given that men with mental health illness and prostate cancer have more aggressive disease compared to those without a mental health illness, an increased incidence of definitive therapy is encouraging.
- However, worse post-treatment surveillance adherence and increased biochemical recurrence rates present an opportunity for interventions to improve outcomes in these patients.
Presented by: Zachary Klaassen, MD, MSc, Associate Professor, Department of Urology, Wellstar MCG Health, Augusta, GA
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, May 31st – June 4th, 2024


