(UroToday.com) The 2024 American Society of Clinical Oncology (ASCO) annual meeting featured a session on prostate cancer, and a presentation by Dr. Stacy Loeb discussing physicians' use of first-line treatment intensification in metastatic castration-sensitive prostate cancer (mCSPC). First-line treatment intensification (i.e. ADT with chemotherapy, novel hormonal therapies, or both) for CSPC is the recommended treatment option in the NCCN Guidelines and the AUA guidelines. However, first-line treatment intensification is only used in <1/3 of patients.
Phase 1 of the IMPLEMENT study used an implementation science approach to identify barriers to and facilitators of treatment intensification. Barriers included knowledge gaps, costs, anticipated regret over exhausting treatment options, and facilitators included knowledge of clinical trial data, a habit of intensifying first-line therapy, interdisciplinary collaboration, and clinical staff support. The goal of Phase 2 of IMPLEMENT was to prioritize these factors and identify resources to increase treatment intensification.
A discrete choice experiment was developed for 300 US-based physicians (150 oncologists and 150 urologists) who manage mCSPC. The trial design for IMPLEMENT is as follows: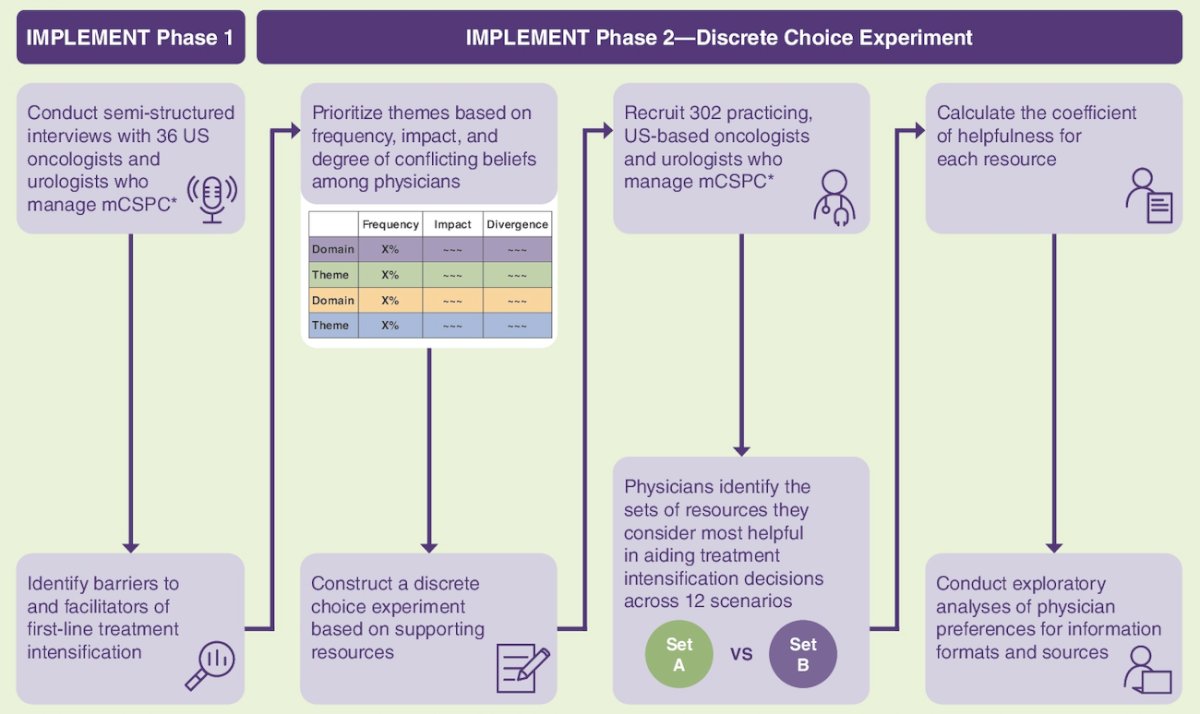
It included 6 descriptions of potential resources to help with treatment intensification decisions, based on results from Phase 1. Physicians were asked to think about the treatment intensification decision challenges they face and to review 12 scenarios to choose one of two resource sets they found most helpful: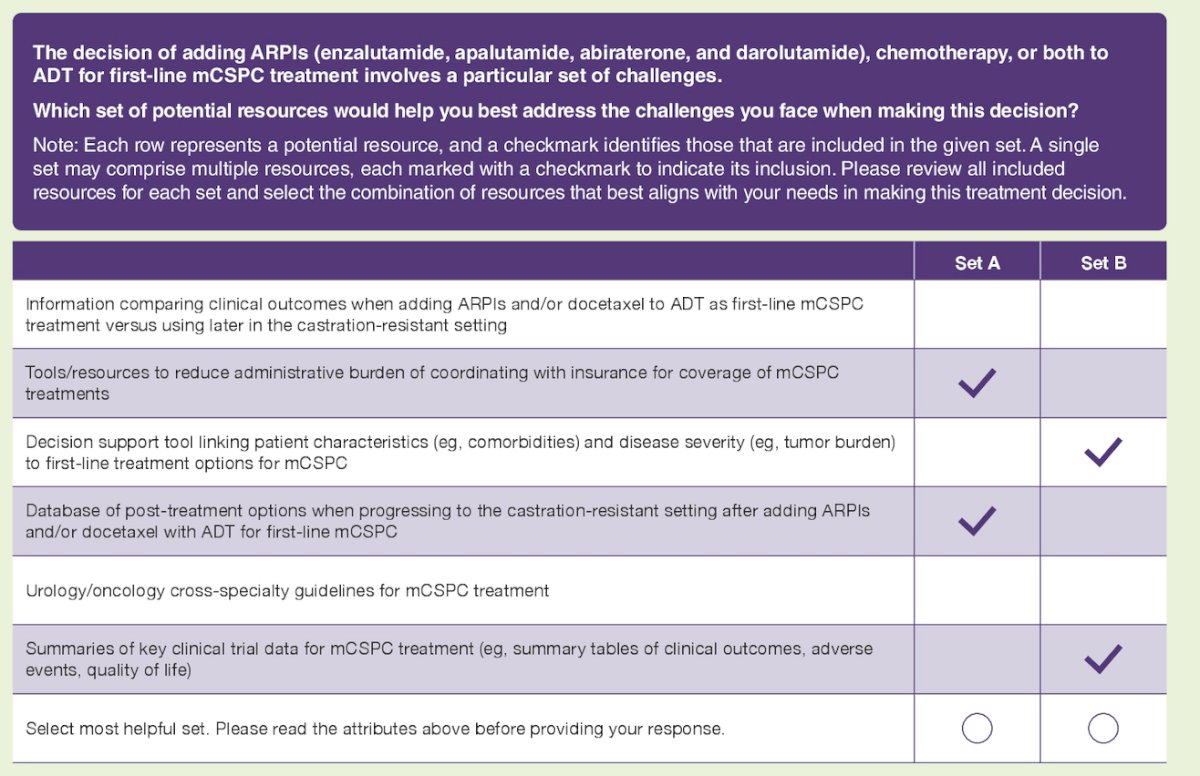
After the discrete choice experiment, respondents adjusted a balance slide between two items on a scale from 1 to 100 to indicate information and practice pattern preference. Dr. Loeb and colleagues then analyzed responses using a mixed-effects logistic regression model and calculated a coefficient of helpfulness for each resource to identify those with the strongest impact on physicians’ decisions. Coefficients were required to have a minimum value of zero, as resources would be optional.
Overall, physicians preferred decision support tools and databases of post-treatment options, with tools to reduce administrative burden considered less helpful. Urologists found decision support tools most beneficial (coefficient of helpfulness 3.27; 95% CI 2.90-3.64), while oncologists preferred post-treatment databases (2.58; 95% CI 2.29-2.89) and clinical trial summaries (2.41; 95% CI 2.13-2.69). Tools to reduce administrative burden and information on outcomes of earlier versus later treatment intensification were not considered as helpful compared to other resources and across specialties.: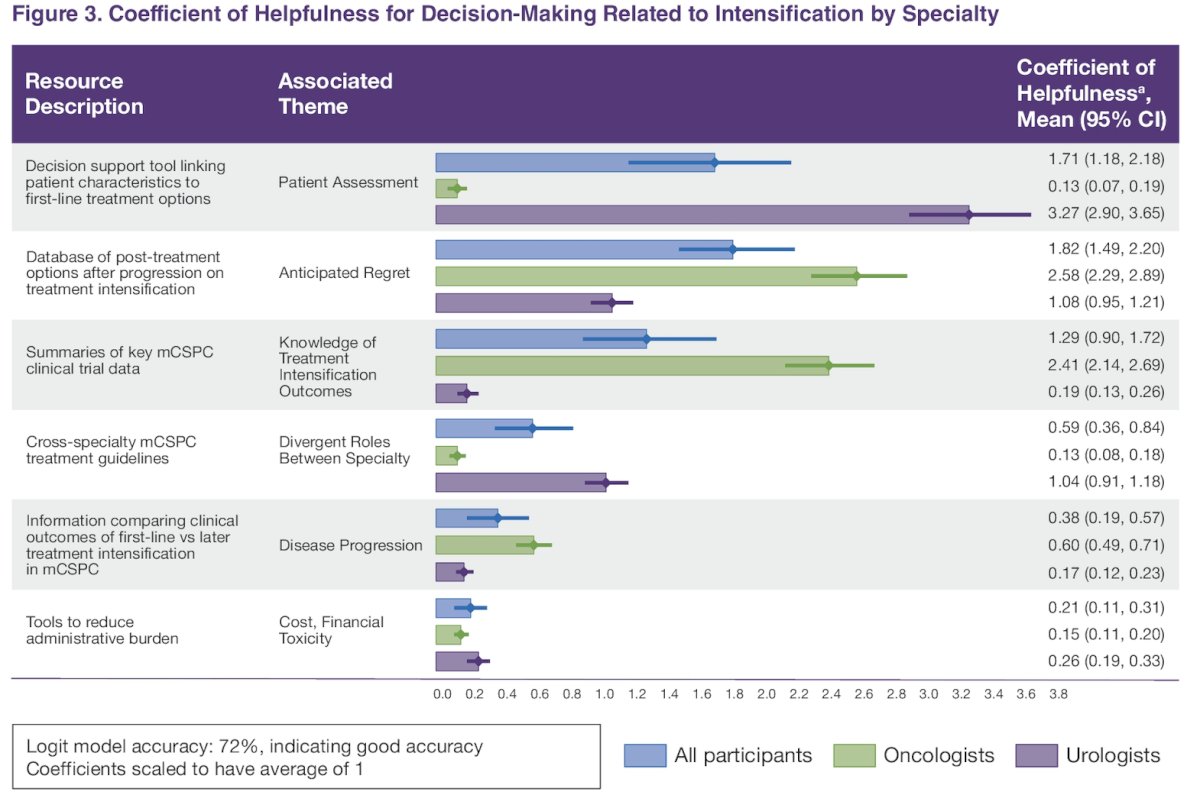
Oncologists had no strong preferences regarding succinctness or directness of information but tended to follow a more individualized approach. Urologists preferred succinct summaries as well as clear and direct information while tending to follow standardized and individualized treatment approaches equally: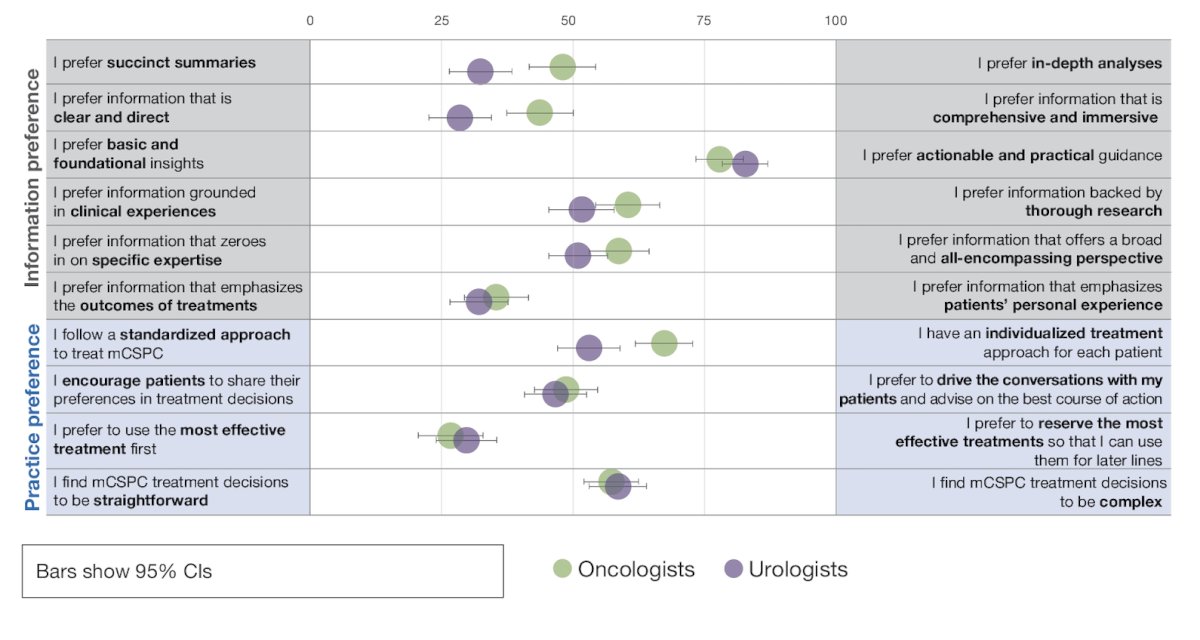
Dr. Loeb concluded her presentation discussing physicians' use of first-line treatment intensification in mCSPC with the following take-home messages:
- There were key differences between specialties in the helpfulness of resources, indicating substantial variability in clinical practice needs
- These findings provide a clear evidence-based path to develop concrete, specialty-tailored tools to increase guideline-concordant treatment intensification for mCSPC
Presented by: Stacy Loeb, MD, Urologic Oncologist, NYU, Langone Health, New York, NY
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, May 31 – Tues, June 4, 2024.


