(UroToday.com) The 2024 American Society of Clinical Oncology (ASCO) annual meeting featured a session on prostate cancer, and a presentation by Dr. Umang Swami discussing the correlation of BMI with survival outcomes in patients with metastatic hormone-sensitive prostate cancer (mHSPC) in the SWOG 1216 study. Obesity has been associated with improved survival outcomes in metastatic castration-resistant prostate cancer.1 However, the association of obesity with survival has not been reported in mHSPC setting. At the 2024 ASCO annual meeting, Dr. Swami and colleagues reported on the correlation of BMI with survival outcomes from patient level data from the phase III SWOG 1216 study,2 which randomized patients with mHSPC in 1:1 to ADT + bicalutamide or ADT + orteronel.
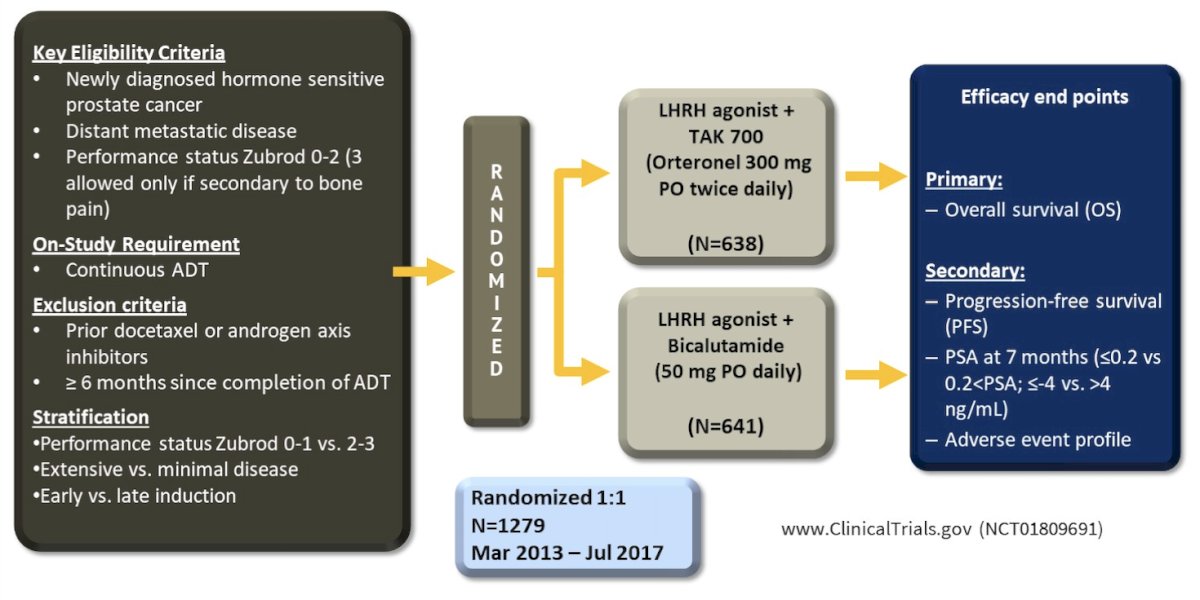
The main inclusion criteria were all patients treated in the SWOG 1216 study with available BMI data. The trial design for the SWOG 1216 study is as follows:
Overall survival was summarized by median survival and 95% CI. Multivariable analysis for overall survival was conducted using Cox proportional hazard model with categorized BMI as a continuous variable and adjusted for treatment arm, disease burden, Gleason score, log PSA, age, and Zubrod performance status.
Among 1,279 patients, 12 were underweight, 252 had normal BMI, 958 were overweight, and 57 were obese. The median age was 67.8 (IQR: 61.9, 73.9) years, 88% of patients had no visceral metastases, and baseline log2 median PSA was 4.89 (IQR: 3.27, 6.76). All four BMI cohorts had similar ages, Gleason scores, extensive disease burden, liver metastases, and treatment allocation (p > 0.05). Differences in baseline PSA and Zubrod performance status were observed between BMI cohorts (p < 0.05):
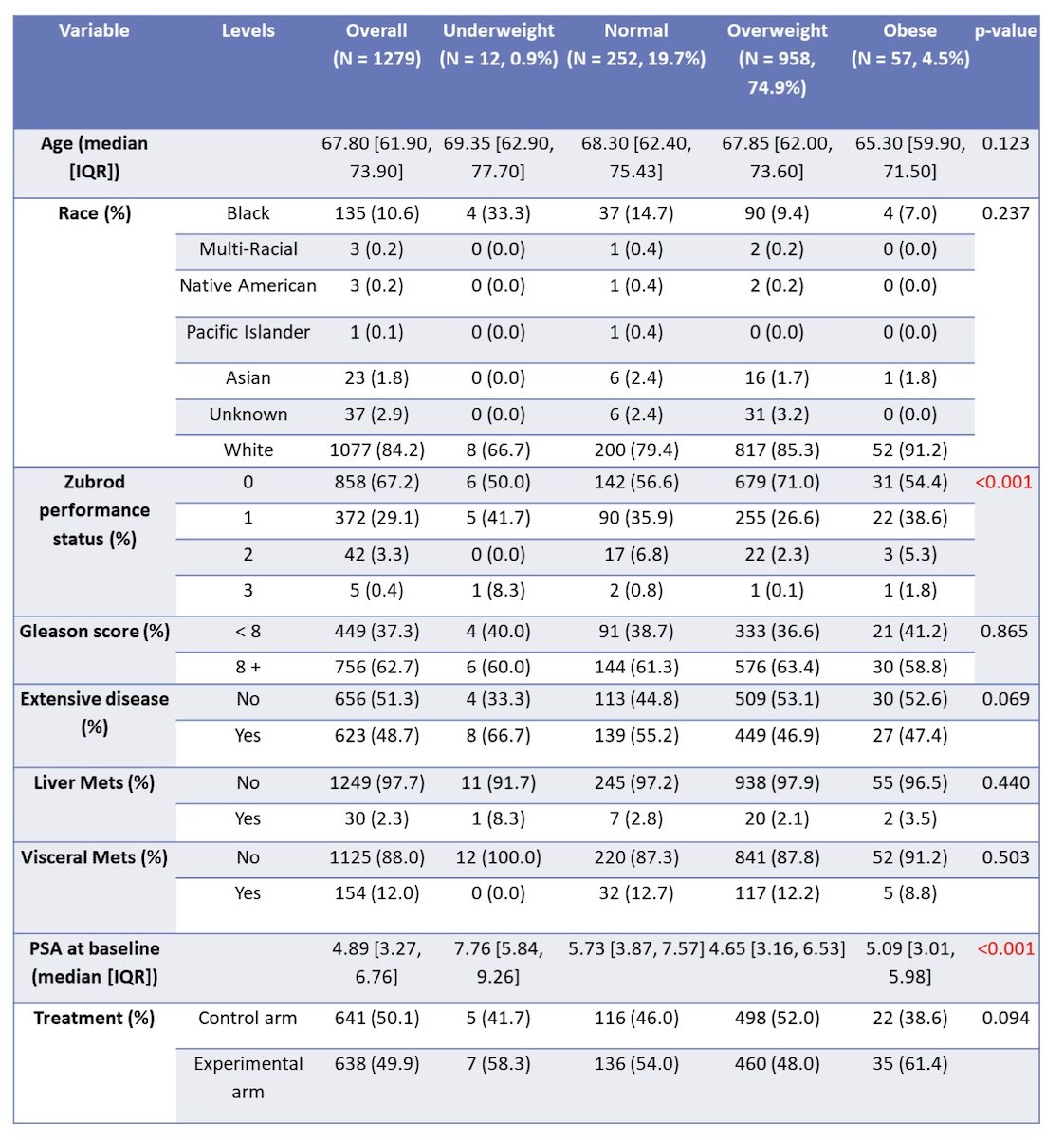
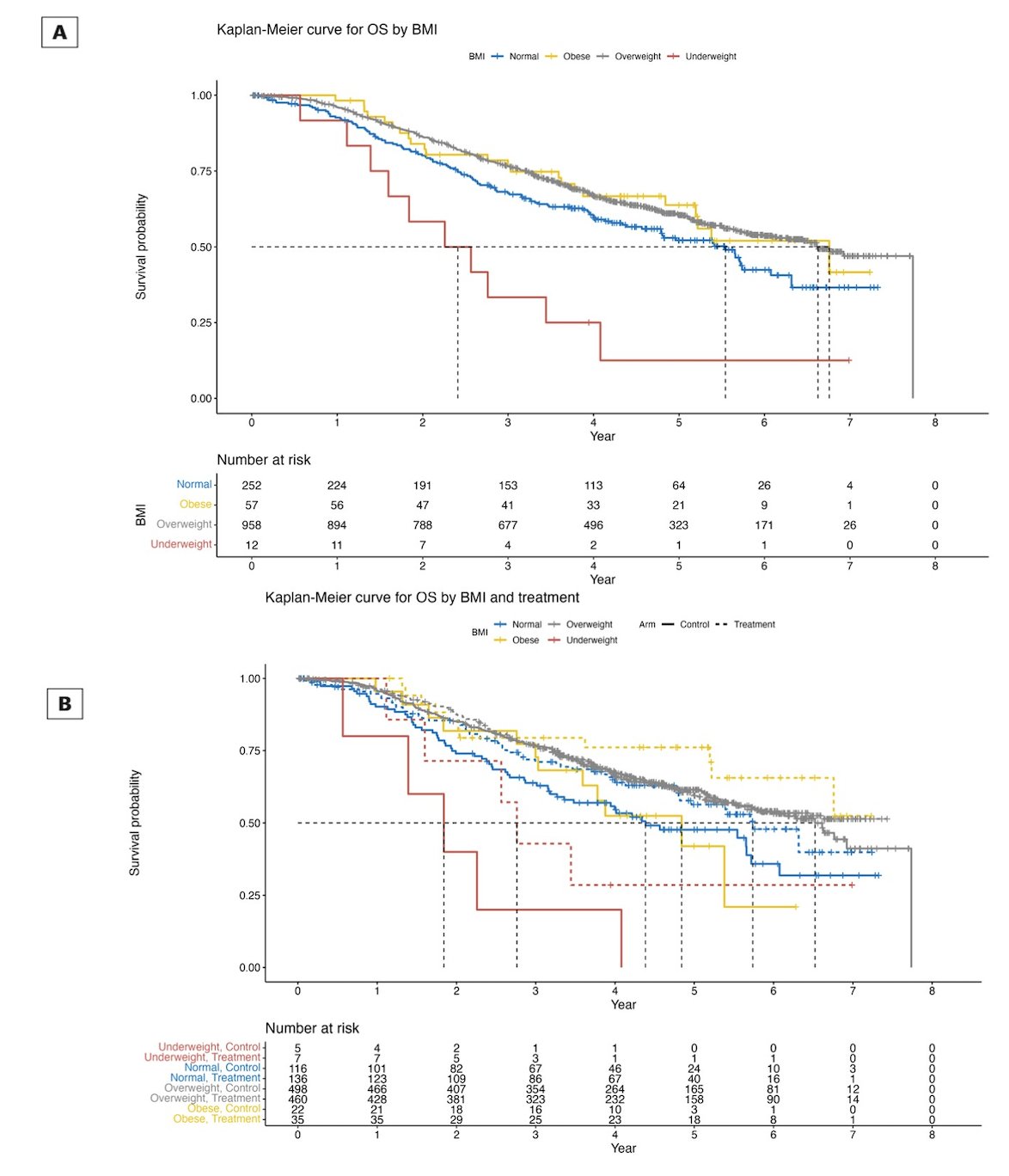
The overall survival in underweight men was 1.8 years, normal weight was 4.4 years, overweight men was 6.5 years, and 4.8 years for obese men in the bicalutamide arm compared to 2.8 years, 5.7 years, not reached, and not reached for orteronel arm, respectively:
After adjusting for prognostic variables, multivariable analysis confirmed that high BMI is associated with better overall survival (HR 0.82, 95% CI 0.68-0.98; p=0.029).
Dr. Swami concluded his presentation by discussing the correlation of BMI with survival outcomes in patients with mHSPC in the SWOG 1216 study with the following take home messages:
- These results show that as categorized BMI increased, the risk of death decreased in patients with mHSPC
- These data warrant external validation in other randomized phase III studies and can help counseling and prognostication of patients with mHSPC in the clinic
Presented by: Umang Swami, MD, Huntsman Cancer Institute at the University of Utah, Salt Lake City, UT
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, May 31st – June 4th, 2024
References:
- Martini A, Shah QH, Waingankar N, et al. The obesity paradox in metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis. 2022 Sep;25(3):472-478.
- Agarwal N, Tangen CM, Hussain MHA, et al. Orteronel for Metastatic Hormone-Sensitive Prostate Cancer: A Multicenter, Randomized, Open-Label Phase III Trial (SWOG-1216). J Clin Oncol. 2022 Oct 1;40(28):3301-3309.


