(UroToday.com) The 2024 American Society of Clinical Oncology (ASCO) Annual Meeting held in Chicago, IL between May 31st and June 4th, 2024 was host to a session addressing techniques to minimize the effects of androgen deprivation therapy (ADT) while explore alternatives in prostate cancer management. Dr. Brian Gonzalez discussed patient-centered approaches to improve quality of life and mitigate the adverse effects of ADT.
Behavioral interventions, such as cognitive behavioral therapy (CBT) and physical activity, can help mitigate adverse effects of ADT, including fatigue, depressive symptoms, and sleep disruption. Behavioral strategies play a critical role in patient-centred clinical practice and can help improve health related quality of life.
ADT has numerous adverse effects that may impact quality of life, including:
- Vascular disorders
- Reproductive system disorders (e.g., impotence and loss of libido)
- General disorders (e.g., sleep disturbances)
- Psychiatric disorders (e.g., depression)
- Metabolic changes (e.g., weight gain)
- Musculoskeletal changes (e.g., muscle atrophy)
The NCCN Survivorship Guidelines recommend behavioral interventions for the management of ADT-related symptoms that:
- Address multiple symptoms simultaneously
- Minimize side effects
- Are associated with a low economic burden
- Actively engage patients
- Improve health-related quality of life
- Enhance patient-centered clinical practice
One such intervention is cognitive behavioral therapy. This is a biopsychosocial approach focused on teaching solution-focused strategies, by:
- Refocusing away from negative thoughts about symptoms towards more realistic, helpful thoughts
- Behavioral activation and exposure to feared experiences.
- Improving health behaviors
- Managing stress
- Optimizing social support
- Increasing self-efficacy
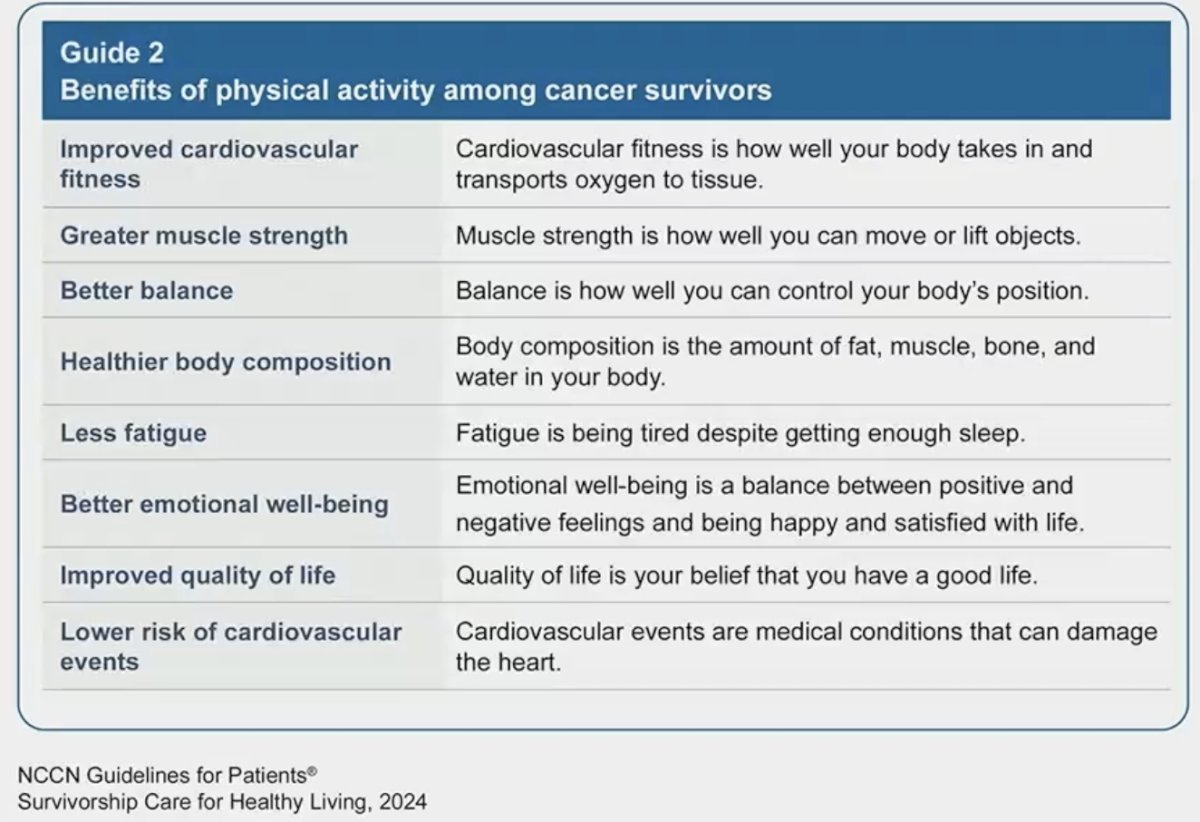
Another important behavioral intervention is physical activity, with the benefits among cancer survivors summarized below.
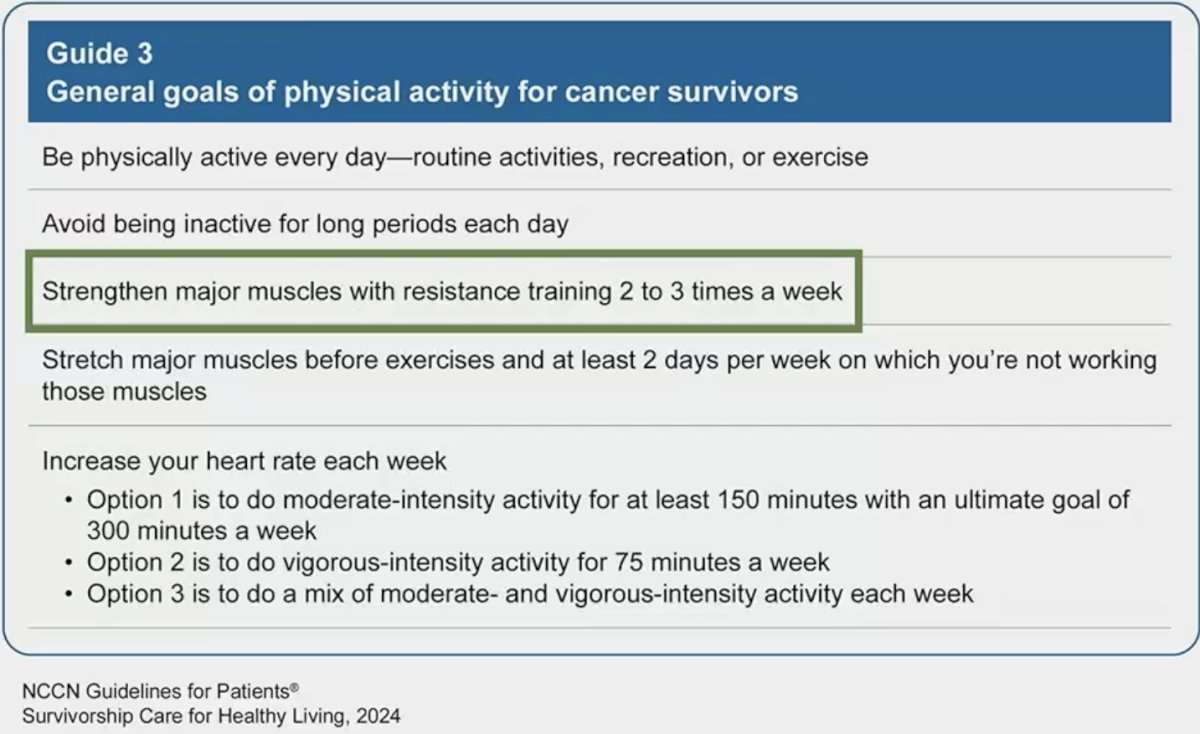
Currently, the 2014 American Cancer Society guidelines for prostate cancer recommend 150 minutes of physical activity per week, without specifying the type. Randomized controlled trials now support combined resistance and aerobic exercise programs in the context of ADT without bone metastases to improve muscle mass, strength, physical function, and balance.1
These behavioral interventions may have synergistic effects by simultaneously targeting/counteracting the adverse effects of ADT, as illustrated below:
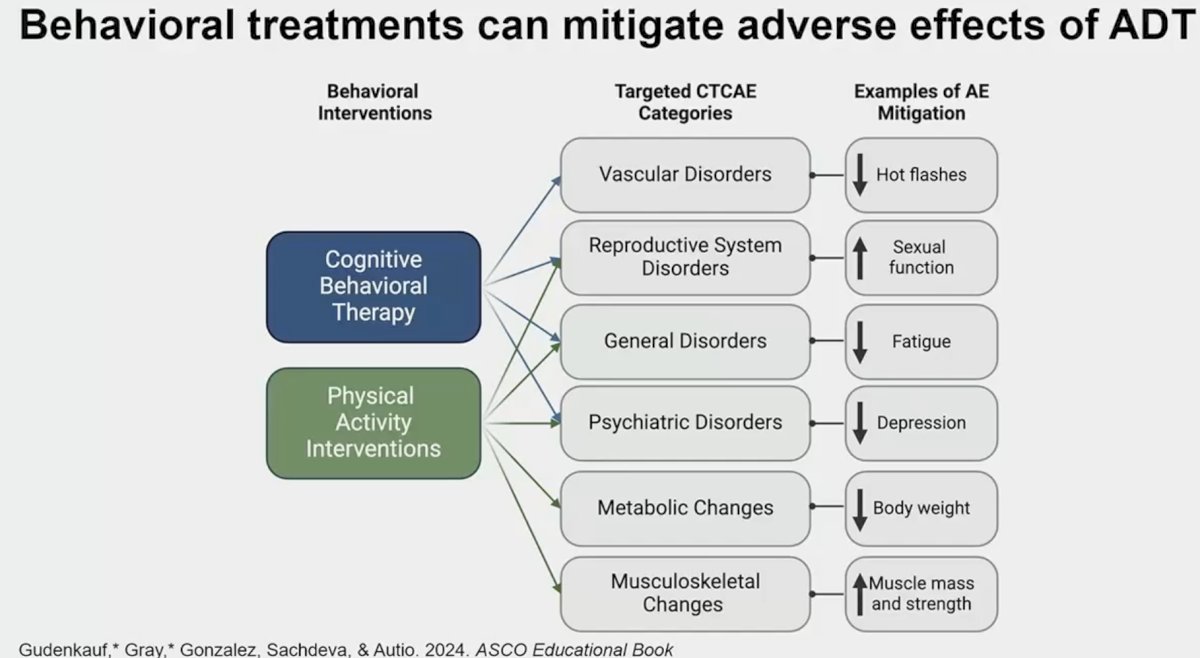
Behavioral treatments can improve health-related quality of life in numerous ways:
- Health promotion: Improve body weight and composition, physical activity levels, and PSA levels
- Physical side effect management: Fatigue, muscle strength, peak oxygen intake, bone health, sexual function, and incontinence.
- Psychosocial functioning: Depression, anxiety, and overall quality of life
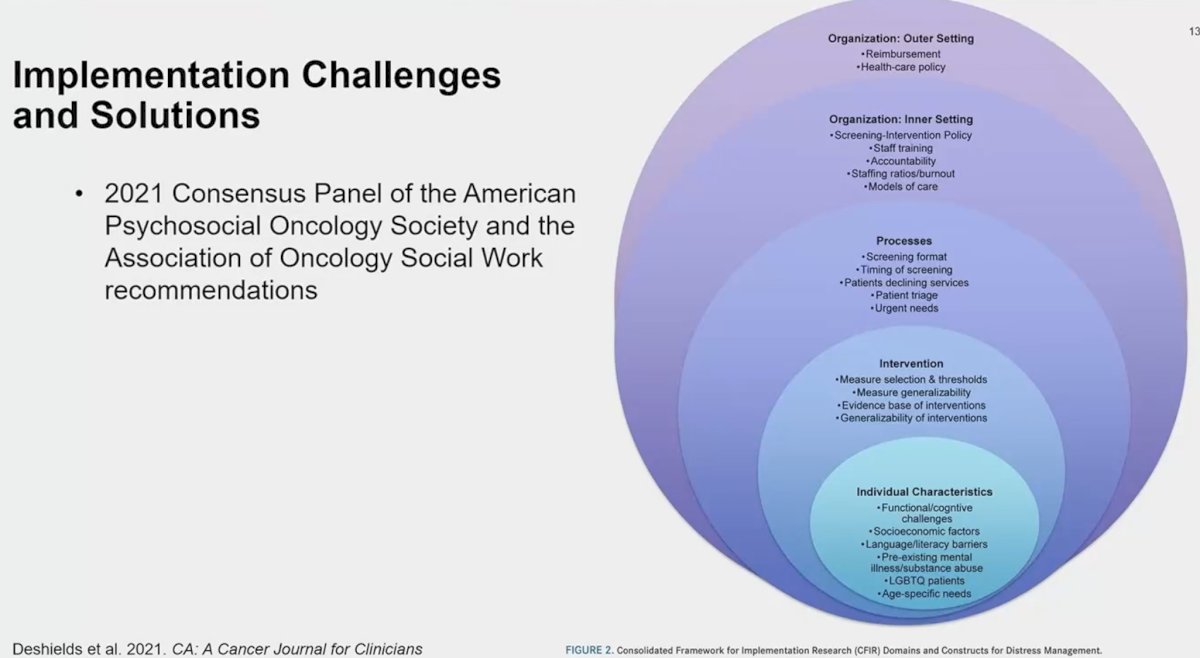
Although the benefits of these behavioral interventions are universally accepted, their adoption in routine clinical practice remains underwhelming. In 2023, Ehlers et al conducted a stakeholder-engaged, mixed-methods, hybrid implementation study to identify barriers to real-world implementation of these behavioral interventions.2 Lack of awareness, both at the physician and patient levels, was an important barrier, as well as clinical practice barriers (e.g., workflow, lack of personnel/skills to provide behavioral training, no specialists available in the community to refer patients to). They proposed the following model for implementing group cognitive behavioral therapy in an interdisciplinary cancer center:
- Stakeholder (physicians/nurses and patients/caregivers) engagement and adaptation of cognitive behavioral therapy delivery
- User testing and adaptation of cognitive behavioral therapy content
- Implementation of adapted cognitive behavioral therapy
Presented By: Brian D. Gonzalez, PhD, Associate Center Director for Research Diversity & Workforce Development, H. Lee Moffitt Cancer Center and Research Institute, Tampa, FL
Written By: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, May 31 – Tues, June 4, 2024
References:
- Sanft T, Day A, Ansbaugh S, et al. NCCN Guidelines® Insights: Survivorship, Version 1.2023. J Natl Compr Canc Netw. 2023;21(8): 792-803.
- Ehlers SL, Gudenkauf LM, Kacel EL, et al. Real-World Implementation of Best-Evidence Cancer Distress Management: Truly Comprehensive Cancer Care. J Natl Compr Canc Netw. 2023;21(6): 627-35.


