The current controversies in sequencing treatments include:
1.Post VEGF inhibitor therapy – should we give a PDL1inhibitor or a different VEGF inhibitor?
2. Post ipilimumab/nivolumab combination therapy or VEGF inhibitor +PDL1 inhibitor should we give:
-VEGF inhibitor vs. mTOR inhibitor?
-Does giving a VEGF inhibitor +PDL1 inhibitor as first-line therapy deprive the patient of a CLTA-4 inhibitor?
-Do we need the best drugs upfront with the highest complete response rates, and best progression-free survival rates, despite having few head to head randomized controlled trials, and not having any cross-trial comparisons?
Dr. Heng continued to discuss the therapeutic options after VEGF therapy. There have been several post VEGF inhibitor randomized controlled trials (Figure 1). Cabozantinib and nivolumab have shown an objective response rate of 20% and 21%, respectively, for these medications given as 2nd line treatments. The median overall survival was shown to be similar in these two medications (7.39 vs.6.9 months, p=0.1983).
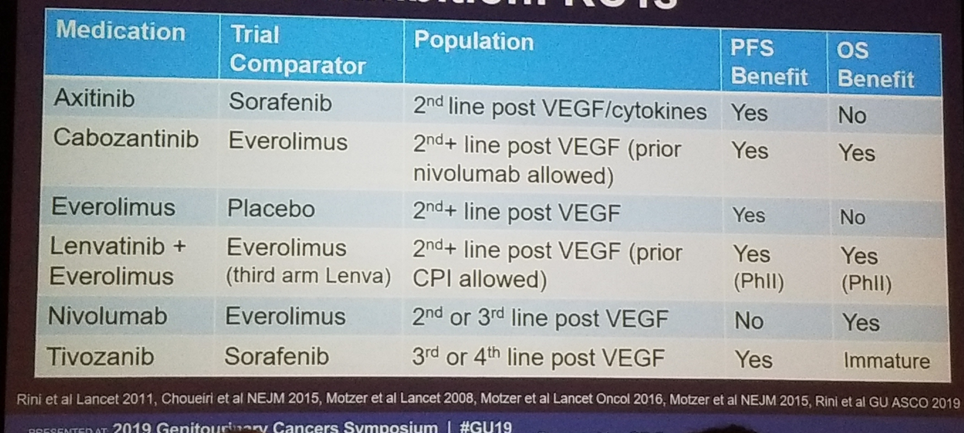
Figure 1 – Post-VEGF inhibition: Randomized controlled trials:
Next, Dr. Heng discussed what is the next treatment for patients who have received prior immune checkpoint inhibitor therapy. There are limited randomized controlled trials looking at this specific subgroup analysis. The two relevant studies are the METEOR study (assessing cabozantinib vs. everolimus after treatment with nivolumab) (Figure 2), and the TIVO-3 trial, which included PD1 treated patients.
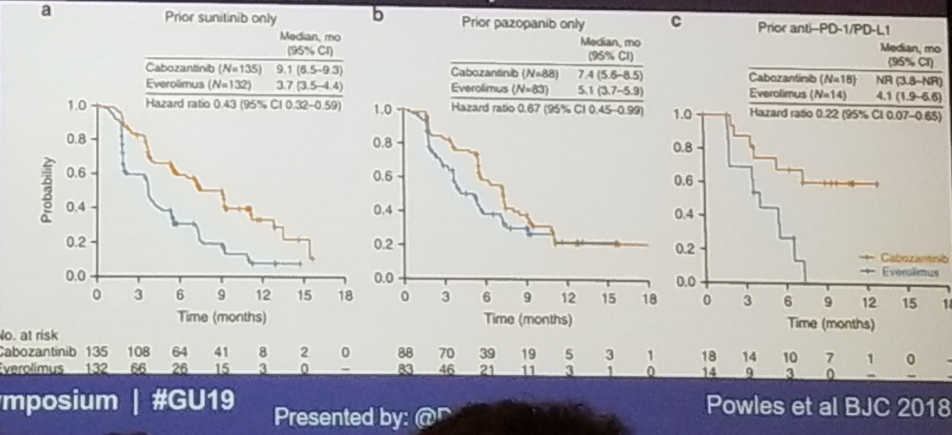
Figure 2- Cabozantinib vs. everolimus following various treatments (METEOR trial):
There is also a phase 2 study, assessing axitinib therapy following immune checkpoint inhibitor. This showed an overall response rate of 39.5% with a median progression-free survival of 9.2 months. It was shown to be well tolerated with 11% grade 3 diarrhea, and 7% grade 3 hand and foot syndrome.
Data presented at ESMO 2018 demonstrated a clear advantage to VEGF inhibitor compared to mTOR following immune checkpoint inhibitor (Figure 3)
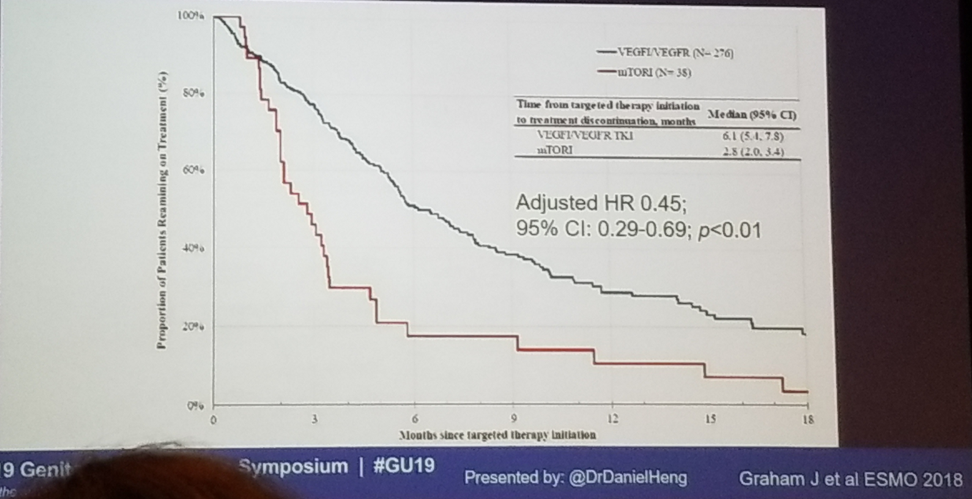
Figure 3 – Post immune checkpoint inhibitor therapy – VEGF better than mTOR:
Currently, there is an international metastatic RCC database consortium, including 10,007 patients from 40 international institutions (figure 4), which facilitates and enables the study of the various sequencing of treatments in a large cohort of patients.
Figure 4 - RCC international database consortium:
Dr. Heng concluded his talk with a summary slide of the possible 2nd and 3rd line therapies after various first-line treatments (figure 5). There is a variety of second-line treatment options. Following immune checkpoint inhibitor therapy, the real-world evidence and prospective trials should guide funding decision. VEGF inhibitors seem to be favored over mTOR in case of prior immune checkpoint inhibitor. There are currently no biomarkers for therapy selection, and this needs to change. The rapid pace of change is most impressive as new therapies emerge constantly.
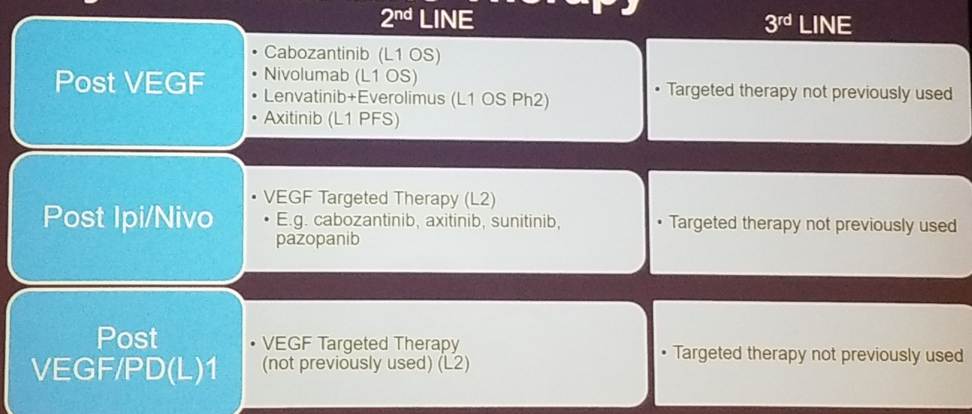
Figure 5 – Beyond first-line therapy:
Presented by: Daniel Yick Chin Heng, MD, MPH, University of Calgary
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre (@GoldbergHanan) at the 2019 American Society of Clinical Oncology Genitourinary Cancers Symposium, (ASCO GU) #GU19, February 14-16, 2019 - San Francisco, CA


