- Remove a large, potentially immunosuppressive tumor that is a potential source of metastases and paraneoplastic syndromes
- Palliate local symptoms of pain or bleeding that could complicate/interrupt systemic therapy
- Obtain accurate pathologic subtyping to guide therapy
- Should never be done to induce spontaneous metastatic tumor regression (it is a real event, but rare)
He also spent time highlighting the highly variable natural history of RCC, as demonstrated in the prior talk by Dr. Samra Turajlic. As a recent paper by Dr. Rini noted (Lancet 2016), some patients with metastatic disease can be watched on surveillance – and can delay systemic therapy safely for > 12 months.
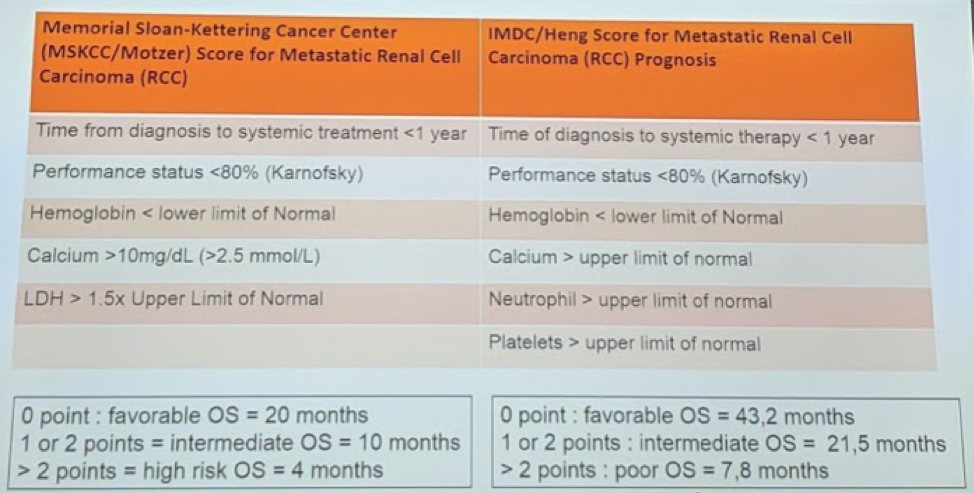
He then briefly reviewed the main risk stratification nomograms to help identify different clinical pathways: the Motzer criteria and the IMDC/Heng criteria.
Since the introduction of targeted therapies in 2006, there has been a reversal in the use of CN. This was seen in a SEER study published in 2013, with a downtrend in CN in mRCC patients. This likely reflects the findings of medical oncologists and even urologists that patients appear to do well with systemic therapy upfront.
More recent retrospective series and meta-analyses in the targeted therapy era have continued to demonstrate a survival benefit to CNx in the setting of mRCC in the targeted therapy age. (Heng et al. EU 2014, Bhindi et al. J Urol 2018) However, this has primarily been in IMDC favorable or intermediate risk patients (IMDC 1-3 risk factors). And, these studies are limited by significant selection bias.
He then briefly reviewed the CARMENA study and its findings.
His main points regarding the CARMENA results:
- Incomplete accrual, underpowered
- Case volume – 79 centers doing on average 0.7 CN/year. None were high volume, and prior studies have demonstrated that this may contribute to oncologic outcomes.
- Poor risk patient enrichment – 43% patients in both arms were poor risk. Most centers already avoid CN in poor risk patients
- ITT design – there was a significant crossover between arms that isn’t captured in an ITT analysis
- Sunitinib is no longer the standard of care for these patients – so the study is already outdated
- Surgical intangibles – data on T-stage, tumor size, the extent of adenopathy, tumor thrombus, and adjacent organ involvement was not included
- Provides local tumor control with an immediate reduction in potentially immunosuppressive tumor burden
- Poor risk patients will NOT benefit in the short term and should undergo biopsy and systemic therapy with consideration of consolidative CN at a later time (if they have good response to systemic therapy).
- With careful case selection and contemporary systemic therapies, OS can now approach 40 months.
- Best if done at high volume centers with substantial medical and surgical back-up to decrease perioperative morbidity and mortality
Presented by: Paul Russo, MD - Memorial Sloan Kettering Cancer Center
Written by: Thenappan Chandrasekar, MD (Clinical Instructor, Thomas Jefferson University) (twitter: @tchandra_uromd, @JEFFUrology) at the 2019 American Society of Clinical Oncology Genitourinary Cancers Symposium, (ASCO GU) #GU19, February 14-16, 2019 - San Francisco, CA
Further Related Content: Questions and Lessons Moving Forward from CARMENA: Which Treatment First? Medical Oncologist’s Perspective


