Dr. Grimm then highlighted the study design and endpoints. The aim was to enroll 1000 (500 per arm) BCG naïve patients with HG Ta-T1 NMIBC +/- CIS. However, recruitment delay due to BCG shortage led to a re-definition of statistical assumptions to 824 patients (412 per arm), prolonged recruitment, and follow-up times. NIMBUS was an international randomized, not blinded trial to establish therapeutic equivalence defined as the lower part of the Confidence Interval (CI) (using one-sided 2.5% level of significance) being higher than a HR (hazard experimental/hazard standard) of 0.75 for recurrence. The treatment arms were: Standard: Induction cycle BCG weekly wks 1-6; maintenance cycles at months 3,6,12 (wks 1,2,3) and Reduced: Induction cycle at wks 1,2,6; maintenance cycles at months 3,6,12 (wks 1,3). Safety was evaluated at yearly intervals by the IDMC, and in case inferiority was shown, defined as the upper part of the CI (one-sided 2.5% level) lower than a HR of 0.75, advice to stop the trial would be given. The primary endpoint was time to the first recurrence. Secondary endpoints were number and grade of recurrent tumors, rate of progression to muscle-invasive disease, safety (treatment-related toxicity > grade 2).

Dr. Grimm then summarized the available data for the IDMC meeting. A total of 345 patients were recruited from Germany (149), the Netherlands (109), France (64), Belgium (22), and Spain (1). Prognostic factors at initial resection were Ta/T1: 46/54%; primary/recurrent disease: 92/8%; single/multiple lesions: 57/43% and concomitant CIS/no CIS: 27/73%. The intention to treat analysis showed a clear difference in time to and number of recurrences between treatment arms: 27% in the reduced arm versus 12% in the standard arm. Known prognostic factors were evenly distributed between arms. Additional safety analyses were performed showing a HR of 0.40 [95% CI: 0.24-0.67]. Early separation of Kaplan Meier survival curves were noted.


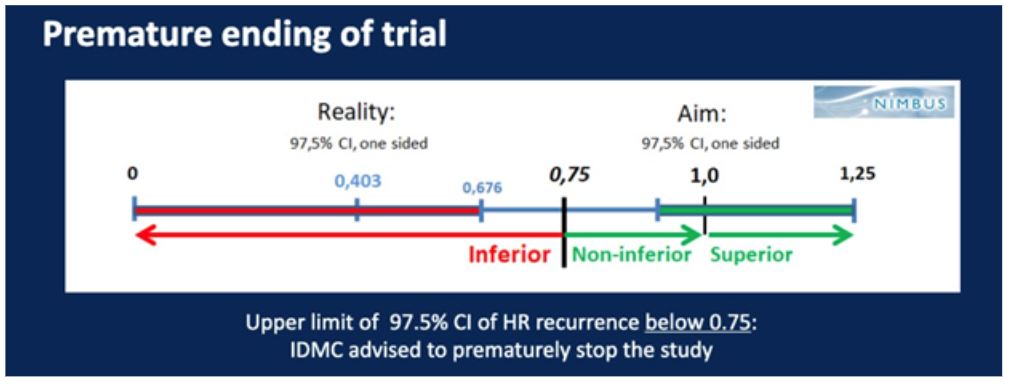
Based on these results, IMDC advised stopping the study prematurely. Patient recruitment was stopped, and patients were informed, and those treated in the reduced arm were given the opportunity to switch to the standard schedule.
Dr. Grimm concluded by noting that in HG NMIBC, a reduced frequency of BCG instillations during induction and maintenance is inferior to the standard BCG-schedule regarding time-to-first-recurrence. In particular, more early recurrences occurred in the experimental arm, suggesting inferior efficacy of the reduced frequency BCG induction schedule. Very few progression events were observed (2%), which may be due to short follow-up time. Fewer patients had adverse events in the reduced frequency arm. The final analysis of NIMBUS with longer follow-up will allow a more mature and detailed analysis. He also stressed that NIMBUS was the first prospective trial using routine re-TUR prior to BCG induction (91% of the patients). The low recurrence and progression rate in the standard frequency arm in a HG NMIBC population (recurrence rate 11% and 15% at 12 and 24 months, respectively) may be attributed to the routine use of re-TUR.
Presented by: Marc-Oliver Grimm, MD, University Hospital, Jena, Germany
Written by: Abhishek Srivastava, MD, Society of Urologic Oncology Fellow, Fox Chase Cancer Center, Fox Chase Cancer Center, Philadelphia, PA @shekabhishek at the 2020 Genitourinary Cancers Symposium, ASCO GU #GU20, February 13-15, 2020, San Francisco, California


