San Francisco, CA (UroToday.com) At ASCO GU 2020, William Y. Kim, MD discussed the molecular subtyping of bladder muscle-invasive urothelial carcinoma.
There is a multitude of molecular subtypes of high-grade muscle-invasive bladder cancer. There has been an effort to try and see if these molecular subtypes can be used as prognostic biomarkers. Studies from various institutions have shown that basal subtype consistently correlates with poor prognosis (Figure 1). Without neoadjuvant chemotherapy, basal subtype has a bad prognosis. Additionally, there is data showing that luminal papillary tumors have a better prognosis (Figure 2). In contrast to the basal subtype, without neoadjuvant chemotherapy luminal subtype has a good prognosis.
Figure 1. Basal subtype consistently correlate with poor prognosis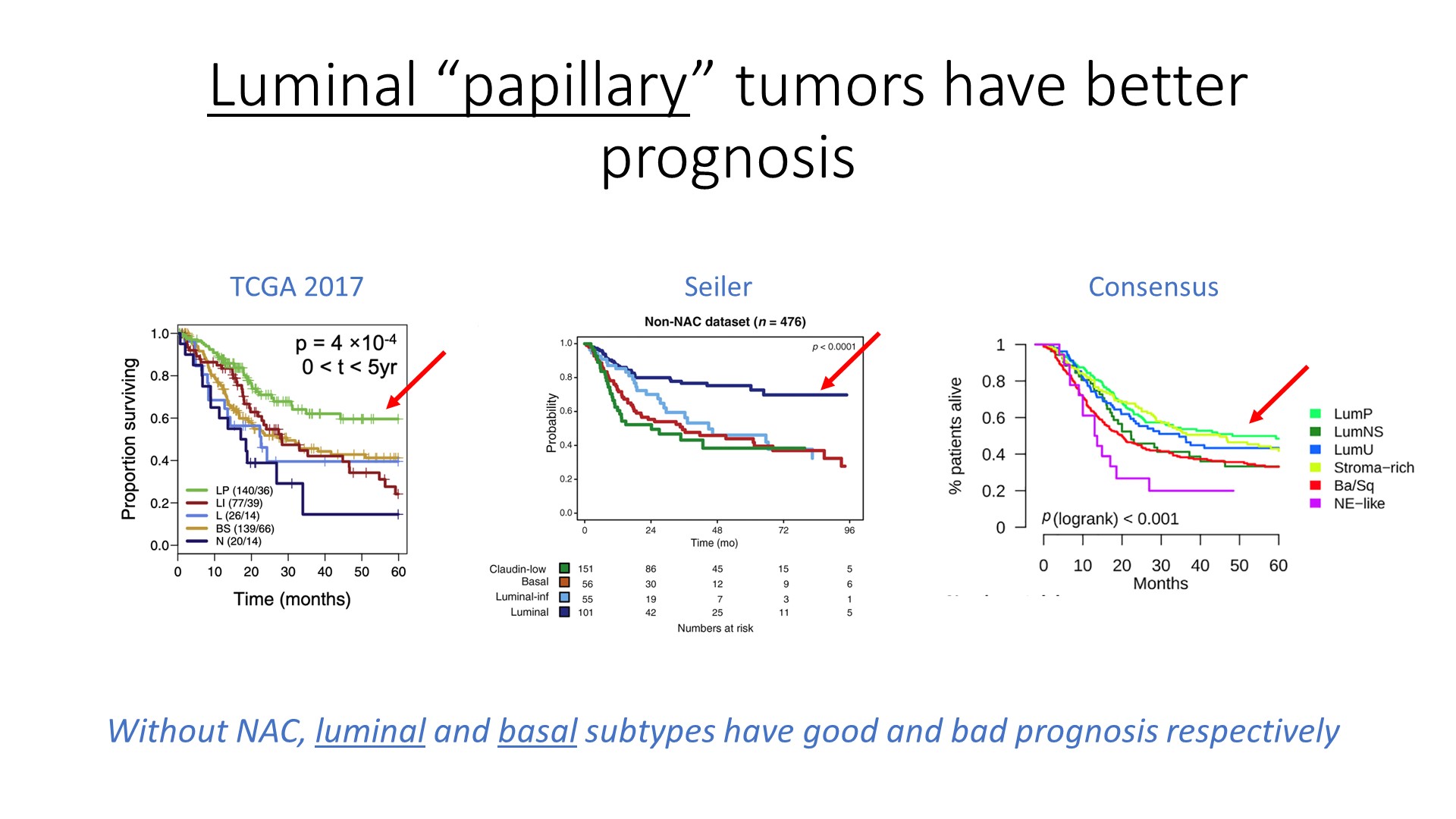
Figure 2. Luminal "papillary" tumors have better prognosis
Dr. Kim moved on to discuss the use of molecular subtypes as predictive biomarkers for neoadjuvant chemotherapy. Basal and luminal tumors have an equivalent response to neoadjuvant chemotherapy (Figure 3). Downstaging from neoadjuvant chemotherapy is associated with improved overall survival in all subtypes except basal tumors (Figure 4).
Figure 3. Basal and luminal tumors have equivalent response to neoadjuvant chemotherapy
Figure 4. Downstaging to neoadjuvant chemotherapy is associate with improved overall survival in all subtypes except basal
It is important to understand that although basal tumors are not downstaged by neoadjuvant chemotherapy, they do have improved survival. This could be explained by the idea that basal urothelial carcinoma could be associated with improved survival after neoadjuvant chemotherapy regardless of downstaging. Possible explanations include the fact that basal bladder tumor actually has higher clinical stage than appreciated (i.e. they actually do have higher downstaging rate). Alternatively, basal tumors may have a dichotomy in the response of primary vs. metastatic sites, where primary tumors may be chemorefractory while metastases may be chemosensitive.
Next, Dr. Kim discussed the role of molecular subtypes as predictive biomarkers for neoadjuvant immune checkpoint blockade. Data on the correlation of subtype to immune-checkpoint response in the metastatic setting remains conflicting. The correlation of subtype to neoadjuvant immune checkpoint inhibitors response has not been extensively explored.
Concluding his talk, Dr. Kim reiterated that molecular subtypes are prognostic. Their clinical utility as a predictive biomarker for neoadjuvant chemotherapy response suggest basal tumors may benefit the most from neoadjuvant chemotherapy. However, these findings require prospective validation. As immune checkpoint blockade and enfortumab vedotin are examined in the neoadjuvant setting, subtype specific response should be examined as well.
Presented by: William Y. Kim, MD, Rush S. Dickson Distinguished Professor of Medicine, Professor of Genetics, UNC Lineberger Comprehensive Cancer Center, Chapel Hill, North Carolina
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New York, Twitter: @GoldbergHanan, at the 2020 Genitourinary Cancers Symposium, ASCO GU #GU20, February 13-15, 2020, San Francisco, California.


