San Francisco, CA (UroToday.com) Based on randomized clinical trials that showed overall survival (OS) advantage with nephrectomy followed by interferon therapy, upfront cyto-reductive nephrectomy has been an option for the treatment of metastatic kidney cancer. Indeed, in rare cases (< 2%), spontaneous regression of metastatic lesions after nephrectomy has been observed. However, in the era of more modern immunotherapy and combination TKI/immunotherapy, the role of cyto-reductive nephrectomy is less clear.
To illustrate the current state of the evidence and his approach, Anil Kapoor, MD, presented the case of a 69-year-old man who developed hematuria and was found to have a left renal mass. Staging imaging revealed two lung metastases. His risk classification was intermediate based on the time from diagnosis to treatment of less than one year. Options that Dr. Kapoor posed to the audience to consider for this patient include upfront left radical cytoreductive nephrectomy, TKI therapy with sunitinib or pazopanib, dual checkpoint blockade with ipilimumab and nivolumab, combination axitinib and pembrolizumab or clinical trial.
Dr. Kapoor then went on to discuss the randomized CARMENA trial, which at face value suggested that for Memorial Sloan Kettering Cancer Center (MSKCC) intermediate/poor risk patients, sunitinib was not inferior with regards to overall survival compared to sunitinib in combination with nephrectomy. Over 40% of patients on trial were poor risk in each arm by MSKCC risk criteria. The trial further showed that median overall survival was longer with sunitinib monotherapy, and that 22.5% of patients never recovered enough after cyroreductive nephrectomy to receive subsequent sunitinib. Therefore, the authors concluded that cytoreductive nephrectomy should no longer be part of standard of care for patients with metastatic RCC requiring medical treatment.
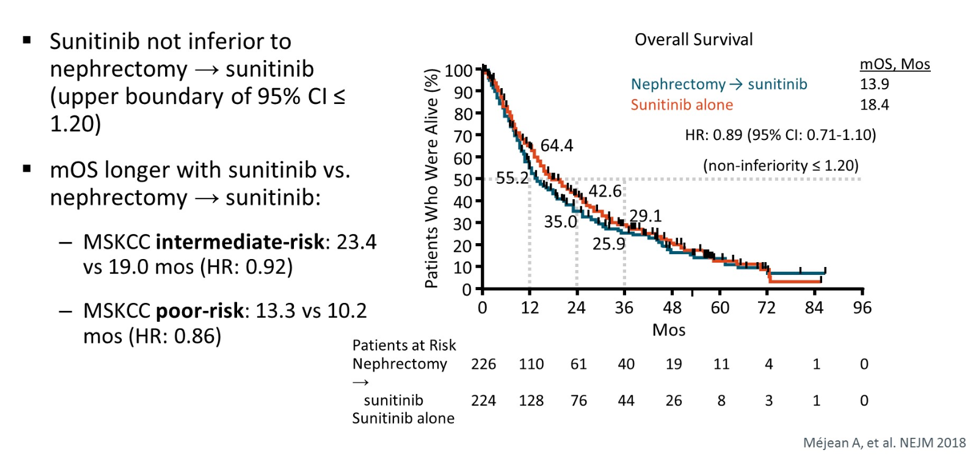
Several caveats to the CARMENA trial were noted. This included incomplete enrollment, possible selection bias in which patients were enrolled on trial since many intermediate-risk patients that were screened were not randomized and patients could be excluded at the investigator’s discretion without disclosure of reason why. Additionally, there was a high percentage of patients with poor risk disease on trial, associated with a relatively short overall survival relative to two prior sunitinib trials.
Regardless, the results of the CARMENA trial continue to hold true, with an update presented at ASCO 2019 showing no difference in overall survival in the intermediate risk group (15.6-month median OS in surgery/TKI group versus 19.8 months in sunitinib alone HR 0.97). Interestingly, 40 patients in the sunitinib monotherapy arm eventually underwent delayed nephrectomy, and these patients did much better in this unplanned subgroup analysis (median OS 48.5 versus 15.7 months, HR 0.34, 95% CI 0.22-0.54). Given the clear selection bias, at best this data is a hypothesis, suggesting that delayed nephrectomy may have some benefit.
To answer the question of immediate versus delayed surgery, the SURTIME trial was undertaken.
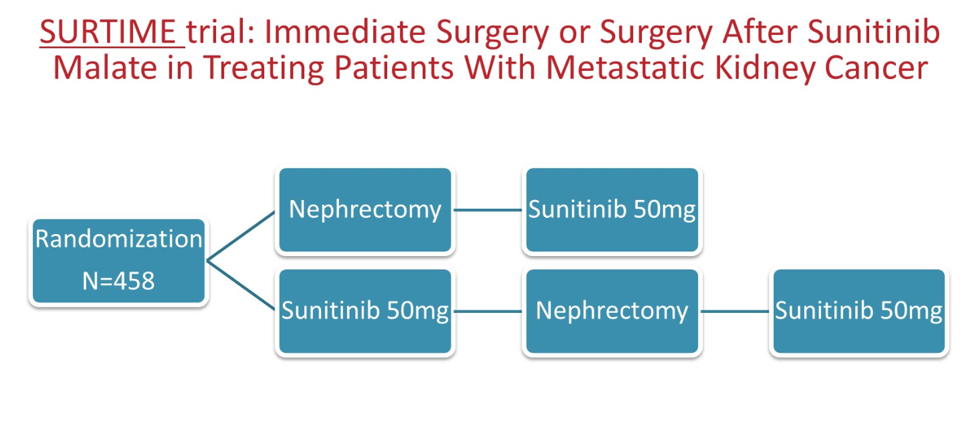
Unfortunately, the trial accrued slowly, with only 99 patients on trial of the planned 458 when data was presented. This exploratory results analysis showed that the sequence of surgery and systemic therapy did not impact progression free survival (PFS) in this patient cohort. It was suggested that a delayed approach could provide a “litmus test” for avoiding surgical harm in patients that ultimately do not do well on systemic therapy.
In summary, there is enough uncertainty in the evidence that guidelines such as those from the Kidney Cancer Research Network of Canada suggest that nephrectomy in metastatic RCC should not be completely abandoned, but rather those patients that undergo this procedure should be carefully selected. Dr. Kapoor noted that patients with lower performance status (ECOG >=2 or KPS < 80) or limited life expectancy (<1 year) should not undergo cytoreductive nephrectomy. Patients with intermediate/poor risk disease, significant symptoms from their disease, active CNS mets, small volume renal disease relative to metastatic disease, or rapidly progressive disease should first receive systemic therapy prior to consideration of nephrectomy. In patients with good performance status, low risk, young age, and relatively minimal symptoms and metastatic disease burden, cytoreductive nephrectomy should be considered upfront. Importantly, CARMENA did not directly address this latter patient population.
Ultimately, Dr. Kapoor emphasized that the decision for cytoreductive nephrectomy should be made within a multidisciplinary discussion, with care not to forget about surgery as a therapeutic modality if indicated. For the case presented at the beginning of the talk, he advocated for either upfront nephrectomy with observation after and treatment if the mets grow OR systemic therapy up front and evaluate for delayed nephrectomy in close follow-up.
Presented by: Anil Kapoor, MD, Professor of Urology, McMaster University, Canada
Written by: Alok Tewari, MD, PhD, Medical Oncology Fellow at the Dana-Farber Cancer Institute, at the 2020 ASCO Genitourinary Cancers Symposium (#GU20), February 13th-February 15th, San Francisco, CA


