San Francisco, CA (UroToday.com) Adjunctive surgery is often without oncological benefit at time of post-chemotherapy retroperitoneal lymph node dissection (PC-RPLND).
The optimal management of post-chemotherapy residual masses for metastatic germ cell tumors (GCT) has long been debated, and several guidelines exist to guide the clinician regarding timing of imaging and the nature of surgery. With particular respect to non-seminomatous germ cell tumors (NSGCT), complete surgical resection (typically PC-RPLND for residual retroperitoneal masses) by surgeons with expertise in the area remains the standard of care. In recent years, large retrospective cohorts have detailed the extent of morbidity regarding these procedures, in particular ‘adjunctive surgery’ – the need for resection of adjacent visceral or vascular organs to achieve completed resection of the residual masses. There is a need to better understand adjunctive surgery in this context. At ASCO GU 2020, Tim Nestler, MD, from the University Hospital of Cologne presented a large retrospective study of adjunctive organ resections.
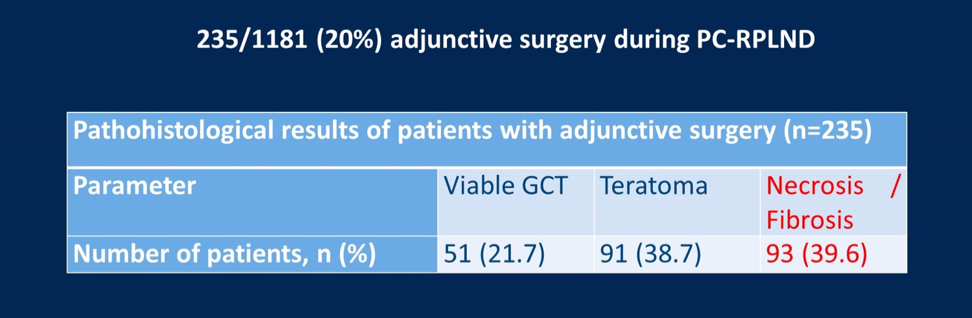
The retrospective 2-center study identified 1181 patients who underwent PC-RPLND between 2008 and 2018. All cases were annotated for the presence of viable tumor, pure teratoma or necrosis/fibrosis. In total 235 (20%) cases of adjunctive surgery during PC-RPLND were noted. Of these cases, 27% underwent resection of multiple organs. The pathology of the 235 patients were reviewed, revealing: 21.% viable germ cell tumor, 39.7% teratoma, 39.6% necrosis/fibrosis.
Dr. Nestler noted that the kidney was the most frequently resected organ, followed by vena cava and partial liver resections. Most of the various organ resections has a rate of necrosis/fibrosis on pathology review of approximately 40%, and slightly higher in liver resections at 54.2%. Furthermore, intra-operative complications occurred in 21% and were more common in those with viable tumor on pathology review (p=0.021).
Patients with evidence of viable GCT had the shortest relapse-free survival. At median follow-up of 22 months, 27% of patients experienced relapse. 5-year relapse-free survival rates were 18% (viable GCT), 54% (teratoma) and 81% (necrosis).
In summarizing these data, Dr. Nestler noted that 20% of PC-RPLND with adjunctive surgery are oncologically unnecessary given the presence necrosis/teratoma. He suggested possible approaches to reduced to include frozen sections during operations, pre-surgical biopsies of bone metastases and more accurate pre-surgical follow-up (including need for better radiomic data and molecular biomarkers to differentiate histology). During the question and answer component of the session, it was noted that, conversely, one could view this data as 60% of cases having evidence of viable GCT or teratoma requiring full resection and that limitations exist with respect to the accuracy of frozen section during complex surgeries. Put together, this study provides important insight into the distribution of histology seen at PC-RPLND with adjunctive surgery and will spur further research in optimizing patient selection.
Presented by: Tim Nestler, MD, Department of Urology, University Hospital of Cologne, Cologne, Germany
Written by: Anis Hamid, MBBS, Medical Oncology Research Fellow at Dana-Farber Cancer Institute and Medical Oncologist, PhD candidate, University of Melbourne, Australia, Twitter: @anis_a_hamid, at the 2020 ASCO Genitourinary Cancers Symposium (#ASCO # GU20), February 13th to 15th, 2020, San Francisco, CA


