San Francisco, California (UroToday.com) Management of localized prostate cancer varies significantly for patients with low, intermediate, and high risk disease. Prostate cancer risk groups are defined in the NCCN criteria as follows: low risk = Gleason 6, PSA < 10, and T1c disease; intermediate risk = Gleason 7, PSA 10-20, or T2 disease; high risk = Gleason 8-10, PSA > 20, or T3/T4 disease. Dr. Adam Kibel, Professor and Chief of Urology at Brigham and Women’s Hospital and Dana-Farber/Brigham and Women’s Cancer Center discussed individualized approaches to the treatment of localized prostate cancer beyond the NCCN criteria outlined above.
In addition to standard clinical criteria (Gleason score, PSA, and clinical T stage), additional factors, such as genetics, genomics, and MRI can help guide treatment selection in localized prostate cancer. The first factor that Dr. Kibel discussed was the impact of genetics on the treatment of low risk localized prostate cancer. Prostate cancer-specific survival among men undergoing active surveillance is 98% at 10 years. Dr. Kibel proposed that genetics could help determine which subset of men are in the 2% of active surveillance patients at risk of dying of prostate cancer. A landmark study by Pritchard CC, et al in the New England Journal of Medicine in 2016 found that 11.8% of men with metastatic prostate cancer have deleterious germline alterations in DNA repair genes.1 A subsequent study of 1211 men on active surveillance looked at rates of germline alterations in ATM, BRCA1, and BRCA2. Only 2% of men had germline alterations. Importantly, Gleason grade progression on repeat biopsy was significantly higher in germline carriers (42% overall and 55% in BRCA2 carriers) compared to 23% for non-carriers.2 These findings suggest that men with germline DNA repair alteration, especially BRCA2, likely are not good candidates for active surveillance and should proceed directly with definitive local therapy.
Prostate MRI is another widely available tool used in the management of localized prostate cancer to risk-stratify patients. Data supporting this practice comes from The PRECISION Trial, which randomized men who were suspected to have prostate cancer, but not yet undergone biopsy to standard transrectal ultrasonography-guided biopsy with or without MRI-targeted biopsy. The primary endpoint was the detection of Gleason 7 prostate cancer or higher, which occurred in 26% of patients who underwent standard biopsy and 38% who had MRI-guided biopsy.3 This led to an interest in utilizing MRI in active surveillance. The ASIST trial randomized 273 men undergoing active surveillance to standard biopsy with or without MRI-guided biopsy. The rates of stage being upgraded were very similar at one year and higher in the standard biopsy arm at two years. Dr. Kibel concluded that MRI likely has value in active surveillance of patients with low risk prostate cancer, and he continues to use it in clinical practice, but that the ASIST Trial raises concerns about overutilization that need to be explored further.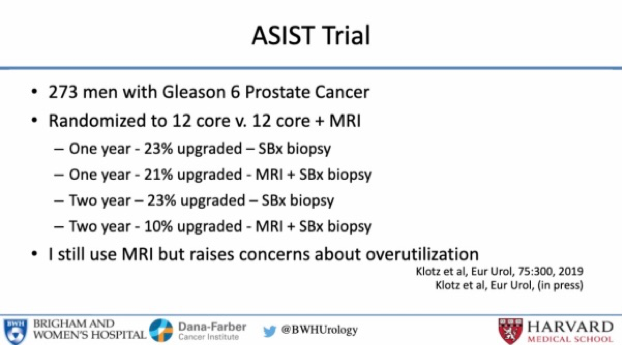
The next topic discussed was whether active surveillance is appropriate for patients with Gleason 7 disease. The slide below highlights the significantly higher rates of metastatic disease in patients with Gleason 4+3 disease making them poor candidates for active surveillance.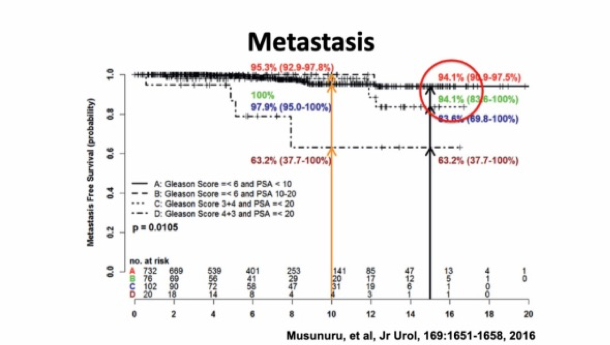
Multiple commercial genomics tests – including Onctotype DX, Decipher, and Prolaris – are available to risk stratify patients based on multi-gene panels. Dr. Kibel focused on a discussion of Decipher but qualified that he does not recommend one test over any of the others. Highlighting data from a publication in Journal of Clinical Oncology, which evaluated how adding Decipher results to NCCN risk score changes management of patients with localized prostate cancer.4 This study found that 44% of favorable-intermediate patients had low-risk genomic scores and thus would be re-classified as low-risk and could be considered candidates for active surveillance. 27% of favorable-intermediate patients had high-risk genomic scores and were re-classified as unfavorable-intermediate, which would necessitate treatment. Of note, no patients with unfavorable-intermediate disease were re-classified to low risk.
Dr. Kibel concluded by briefly discussing men with localized high-risk prostate cancer highlighting superior outcomes for those treated with multi-modality therapy compared to surgery or radiation alone.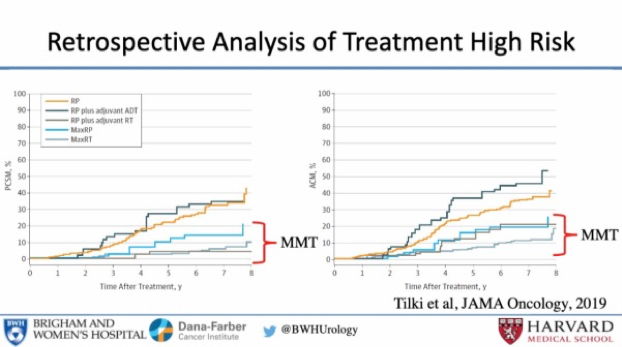
Presented by: Adam Kibel, MD, Professor and Chief of Urology at Brigham and Women’s Hospital and Dana-Farber/Brigham and Women’s Cancer Center
Written by: Jacob Berchuck, MD, Medical Oncology Fellow at the Dana-Farber Cancer Institute (Twitter: @jberchuck) at the 2020 Genitourinary Cancers Symposium, ASCO GU #GU20, February 13-15, 2020, San Francisco, California
References:
- Pritchard CC, et al. DNA-Repair Gene Mutations in Metastatic Prostate Cancer. N Engl J Med 2016; 375:1802-1805. DOI: 10.1056/NEJMc1611137
- Carter HB, et al. Germline Mutations in ATM and BRCA1/2 Are Associated with Grade Reclassification in Men on Active Surveillance for Prostate Cancer. Eur Urol. 2019 May;75(5):743-749.
- Kasivisvanathan V, et al. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N Engl J Med. 2018 May 10;378(19):1767-1777.
- Spratt DE, et al. Development and Validation of a Novel Integrated Clinical-Genomic Risk Group Classification for Localized Prostate Cancer. J Clin Oncol. 2018 Feb 20;36(6):581-590.


