San Francisco, California (UroToday.com) Dr. Richard Lee discussed the topic of novel imaging in the setting of metastatic prostate cancer. He began debating the question of why we need next generation imaging. In the setting of biochemical recurrence novel imaging will allow us to detect disease that is not captured by conventional imaging. It would also allow us to improve the risk assessment and prognostication. Lastly, it will help us drive clinical management and improve patient care. However, a key question we need to answer is whether enhanced detection of metastatic disease improves outcomes as well.
The conventional imaging that has been used in the past include CT/MRI and bone scan. CT and MRI scans give high resolution anatomic details and are widely available. Their main limitation is that they show structure but do not show activity. The sensitivity and specificity for nodal metastasis with lymphadenectomy as a reference guide, show 42% and 82% respectively, for CT scans, and 39% and 82%, respectively, for MRI.
Bone scans allow direct imaging of bone turnover. However, they are prone to subjective interpretation and attempts to quantify have significant limitations. With the PSA level between 0 to 10, a bone scan will be positive in only 4% of cases. When the PSA is between 10 and 20, the bone scan will be positive in 36% of cases, and when the PSA is between 20.1 and 50 the bone scan will be positive in 50% of cases.1 Another important limitation is that when a bone scan is positive, it ultimately requires additional modality imaging to accurately understand what the lesion is.
Next generation imaging involves the usage of one of several molecules. These include Fluciclovine, sodium fluoride, choline, acetate, and PSMA. Dr. Lee Elaborated on the use of Pet/CT Fluciclovine. It has been FDA approved since 2016 and is available in the US. It has an overall detection rate of 67.7% and when the PSA is less than 0.79 it can detect 41.4% of metastatic lesions. When the PSA above 6 it can detect 87% of metastatic lesions. It has been shown to detect more lesions compared with conventional imaging. When compared to CT scans in a trial assessing 53 patients with a median PSA of 4, positive scans were found in 77.4% of the fluciclovine scans compare to 18.9% of the CT scans.2 PET/CT with Fluciclovine has also been shown to have a significant impact on management, with 57% of patients showing the lesion and 59% of them undergoing a change in management as a result of this.3 There have been several studies showing the usage of PET CT with fluciclovine (Table 1).
Table 1 – PET/CT Fluciclovine trials:
Next, PSMA PET/CT imaging was briefly discussed. PSMA is a transmembrane protein expressed in 90 to 95% of prostate cancer cases. There have been multiple ligands that have been used. The scan is currently not commercially available in the US and it has not yet been FDA approved. PSMA PET/CT has shown to change management in 43% of cases compared to conventional imaging. There have been several trials assessing its impact on various PSA levels showing promising results (Table 2).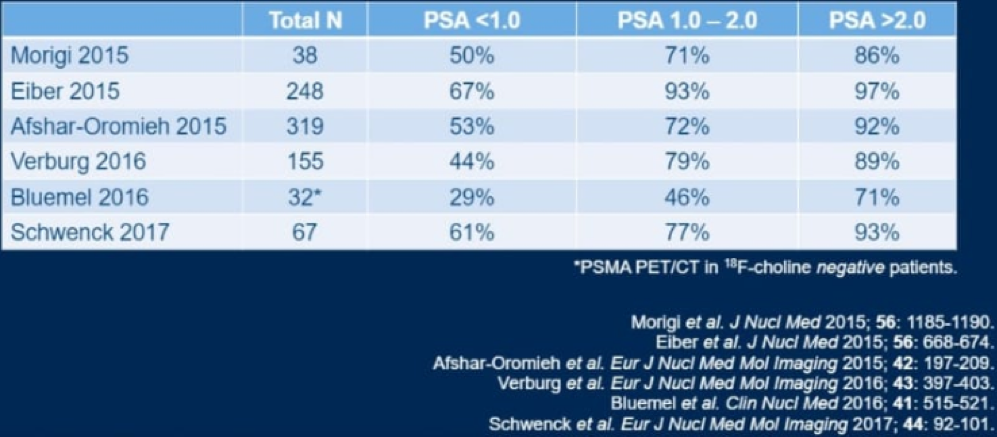
Table 2 – PSMA studies:
When comparing PSMA to Fluciclovine, it seems PSMA has better detection rates with an overall detection rate of 56% compared to 26% , while for pelvic nodes it was 30% compared to 8%, and for extra pelvic M1 disease it was 16% versus 0%.4
It is clear that the introduction of PET scanning with novel molecular imaging offers a greater detection rate at a lower PSA level for PSA recurrence disease (Table 3).
Table 3 – Better results for novel imaging at low PSA levels:
Concluding his talk Dr. Lee stated that newer agents are already here and incorporated in the NCCN and ASCO guidelines. PET scans influence care and may improve local control. The resulting management changes impact the use of radiation and androgen deprivation therapy. However, the most important question of whether advanced imaging improve survival has not been answered yet.
Presented by: Richard J. Lee, MD Professor of Stem Cell and Regenerative Biology at Harvard Medical School, Boston, Massachusetts
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, NY, USA @GoldbergHanan at the 2020 Genitourinary Cancers Symposium, ASCO GU #GU20, February 13-15, 2020, San Francisco, California
References:
- Dotan ZA, Bianco FJ, Jr., Rabbani F, et al. Pattern of prostate-specific antigen (PSA) failure dictates the probability of a positive bone scan in patients with an increasing PSA after radical prostatectomy. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2005; 23(9): 1962-8.
- Odewole OA, Tade FI, Nieh PT, et al. Recurrent prostate cancer detection with anti-3-[(18)F]FACBC PET/CT: comparison with CT. European journal of nuclear medicine and molecular imaging 2016; 43(10): 1773-83.
- Andriole GL, Kostakoglu L, Chau A, et al. The Impact of Positron Emission Tomography with 18F-Fluciclovine on the Treatment of Biochemical Recurrence of Prostate Cancer: Results from the LOCATE Trial. The Journal of urology 2019; 201(2): 322-31.
- Calais J, Ceci F, Eiber M, et al. 18F-fluciclovine PET-CT and 68Ga-PSMA-11 PET-CT in patients with early biochemical recurrence after prostatectomy: a prospective, single-centre, single-arm, comparative imaging trial. The Lancet Oncology 2019; 20(9): 1286-94.


