In the preoperative setting for risk stratification, Dr. Fossati selected the paper by Zelic et al. predicting prostate cancer death with different pretreatment risk stratification tools.1 The objective of this study was to systematically compare the prognostic performance of the most commonly used pretreatment risk stratification tools for prostate cancer using the Prostate Cancer data Base Sweden (PCBaSe) 4.0 among 154,811 diagnosed with nonmetastatic prostate cancer during 1998-2016 and followed through 2016. The authors compared the D'Amico, National Institute for Health and Care Excellence (NICE), European Association of Urology (EAU), Genito-Urinary Radiation Oncologists of Canada (GUROC), American Urological Association (AUA), National Comprehensive Cancer Network (NCCN), and Cambridge Prognostic Groups (CPG) risk group systems, the Cancer of the Prostate Risk Assessment (CAPRA) score, and the Memorial Sloan Kettering Cancer Center (MSKCC) nomogram in predicting prostate cancer death by estimating the concordance index (C-index) and the observed versus predicted cumulative incidences at different follow-up times. Among 139,515 men included in the main analysis, 15,961 died from prostate cancer during follow-up. The C-index at 10 years of follow-up ranged from 0.73 (95% confidence interval [CI] 0.72-0.73) to 0.81 (95% CI 0.80-0.81) across the compared tools. The MSKCC nomogram (C-index: 0.81, 95% CI: 0.80-0.81), CAPRA score (C-index: 0.80, 95% CI: 0.79-0.81), and CPG system (C-index: 0.78, 95% CI: 0.78-0.79) performed the best. The predicted cumulative incidences were close to the observed ones, with some underestimation at 5 years. According to Dr. Fossati, the clinical implications of this study are more personalized treatment decisions and to improve comparability across studies. The strength of this study is that it is a population-based cohort with a large number of events; the limitation is that there is incomplete information for some of the predictors.
The second paper Dr. Fossati selected was by Barzi et al. assessing the influence of facility caseload on the subsequent survival of men with localized prostate cancer undergoing radical prostatectomy.2 The authors used the National Cancer Database to investigate the outcomes of radical prostatectomy in the United States. With overall survival (OS) as the primary outcome, the relationship between the facility annual caseload for all prostate cancer encounters and the facility annual surgical caseload for those requiring radical prostatectomy was examined with a Cox proportional hazards model. Four volume groups were defined by caseload: <50th percentile, 50th to 74th percentiles, 75th to 89th percentiles, and ≥90th percentile. Between 2004 and 2014, 488,389 patients underwent radical prostatectomy. At a median follow-up of 61 months, the median OS was not reached. There was a significant OS benefit as the caseload increased. For facility annual caseload, the adjusted OS difference between the <50th percentile and ≥90th percentile at 90th percentile survivorship reached 13.2 months (hazard ratio [HR] 1.30, 95% CI, 1.23-1.36; p < .0001). For facility annual surgical caseload, this was 11.3 months (HR 1.25, 95% CI, 1.192-1.321; p < .0001).

Dr. Fossati notes that the implications of this paper are that there should be a consideration for the regionalization of radical prostatectomy. The strength of this paper is the population-based cohort and a large number of patients and events. The limitation of this study is the retrospective nature and the inherent selection bias.
The next paper Dr. Fossati selected for surgical technique was the study by Porpiglia et al. that assessed three-dimensional elastic augmented-reality robot-assisted radical prostatectomy using hyperaccuracy three-dimensional reconstruction technology.3 This was a prospective study enrolling 40 patients with prostate cancer undergoing robotic prostatectomy; patients underwent 3D augmented reality (AR) robotic prostatectomy or, in case of unavailability of this technology, 2D cognitive robotic prostatectomy. In all patients, total anatomical reconstruction was used. Twenty patients were enrolled in each group. Focusing on the 3D AR group at macroscopic evaluation, the metallic clip was placed at the tumor and capsular bulging in all cases. At the microscopic assessment, cancer presence was confirmed in the suspicious area in 95.4% of the cases. Moreover, capsular involvement was correctly identified in 100% of the cases, thanks to the 3D image overlap. These results were compared with the 2D MRI cognitive group, showing, at microscopic analysis, statistically significant superiority of the 3D AR group in capsular detection during the nerve-sparing phase (100% vs 47.0%; p<0.05). According to Dr. Fossati, the clinical implications are to improve functional outcomes and reduce the risk of positive surgical margins. The strength of this study is the 3D real-time modulation, whereas the limitations are the time and cost-effectiveness, as well as the small number of patients included.
The next paper Dr. Fossati selected was regarding salvage radical prostatectomy by Marconi et al. published in European Urology.4 This study included a multicenter cohort study of 82 patients undergoing salvage robotic prostatectomy after focal therapy. The type of focal therapy prior to salvage robotic prostatectomy is as follows: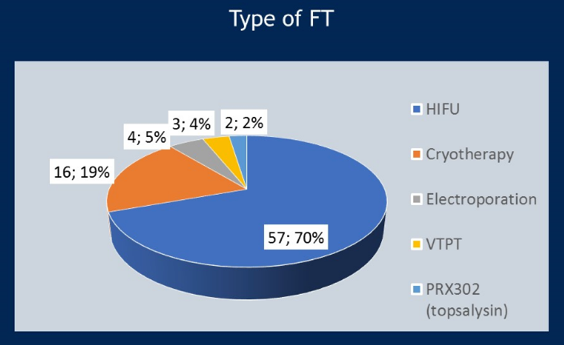
Progression-free survival was 74% at 12 months, 48% at 24 months, and 36% at 36 months after surgery. The 12-month continence rate was 83%. There were no intraoperative complications and no major postoperative complications. On multivariable analysis, only infield recurrence (HR 3.77, 95% CI 1.11-12.85; p=0.03) and pT3b stage (HR 5.0, 95% CI 1.53-16.39; p=0.008) were independent predictors of recurrence. The implications of this study are that we now have outcomes regarding salvage robotic prostatectomy after focal therapy. The strength of this study is that this is the largest series of patients with salvage robotic prostatectomy after focal therapy, whereas the limitation is the retrospective nature and non-comparative design.
The study Dr. Fossati selected for staging after biochemical recurrence was by Jeremie Calais assessing fluciclovine PET-CT and PSMA PET/CT with early biochemical recurrence.5 This study at UCLA assessed patients undergoing 18F-fluciclovine (reference test) and PSMA (index test) PET-CT scans within 15 days. Detection rate of biochemical recurrence at the patient level and by anatomical region was the primary endpoint. Among 143 patients screened for eligibility, of whom 50 patients were enrolled, the median follow-up was 8 months (IQR 7-9). The primary endpoint was met in that detection rates were significantly lower with 18F-fluciclovine PET-CT (13 [26%; 95% CI 15-40] of 50) than with PSMA PET/CT (28 [56%; 41-70] of 50), with an OR of 4.8 (95% CI 1.6-19.2; p=0.0026) at the patient level.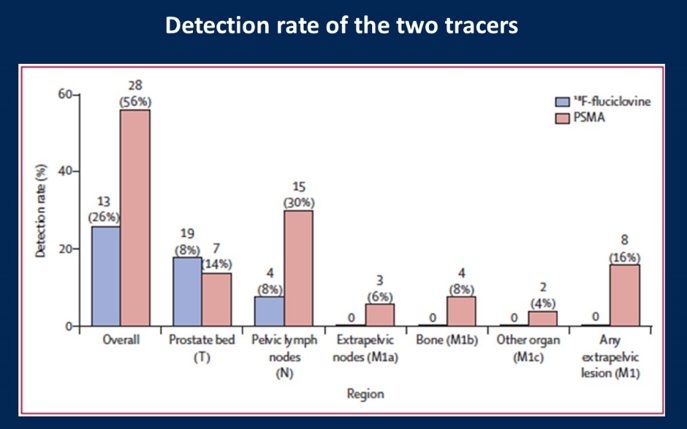
The implications of the current study are that PSMA PET/CT detects sites of recurrence earlier, which may have implications on hard clinical endpoints. The strength of the study is the prospective head-to-head comparison, whereas the limitation is the technical parameters of 18F-fluciclovine and no histological correlation.
The final study Dr. Fossati selected was a quality of life study assessing patient-reported outcomes through five years of active surveillance, surgery, brachytherapy or external beam radiation with or without androgen deprivation therapy for localized prostate cancer.6 This was a prospective, population-based cohort study of 1,386 men with favorable-risk (clinical stage cT1 to cT2bN0M0, PSA ≤20 ng/mL, and Grade Group 1-2) prostate cancer and 619 men with unfavorable-risk (clinical stage cT2cN0M0, PSA of 20-50 ng/mL, or Grade Group 3-5) prostate cancer diagnosed in 2011 through 2012. For men with favorable-risk prostate cancer, nerve-sparing prostatectomy was associated with worse urinary incontinence at 5 years (adjusted mean difference, -10.9 [95% CI, -14.2 to -7.6]) and sexual function at three years (adjusted mean difference, -15.2 [95% CI, -18.8 to -11.5]) compared with active surveillance. Low-dose-rate brachytherapy was associated with worse urinary irritative (adjusted mean difference, -7.0 [95% CI, -10.1 to -3.9]), sexual (adjusted mean difference, -10.1 [95% CI, -14.6 to -5.7]), and bowel (adjusted mean difference, -5.0 [95% CI, -7.6 to -2.4]) function at one year compared with active surveillance. EBRT was associated with urinary, sexual, and bowel function changes not clinically different from active surveillance at any time point through five years. For men with unfavorable-risk disease, EBRT with androgen deprivation therapy (ADT) was associated with lower hormonal function at six months (adjusted mean difference, -5.3 [95% CI, -8.2 to -2.4]) and bowel function at one year (adjusted mean difference, -4.1 [95% CI, -6.3 to -1.9]), but better sexual function at five years (adjusted mean difference, 12.5 [95% CI, 6.2-18.7]) and incontinence at each time point through five years (adjusted mean difference, 23.2 [95% CI, 17.7-28.7]), than prostatectomy. According to Dr. Fossati, the clinical implications are that the 5-year cancer-specific survival is close to 100% for localized prostate cancer, and the functional outcomes and quality of life are the main outcome of interest. The strength of the current study is that robotic radical prostatectomy, IMRT, and risk-based ADT were all included. The limitation of the current study is selection bias, no information after a 5-year follow-up, and no data about investigational strategies (ie. cryoablation, and high-dose brachytherapy.
Presented by: Nicola Fossati, MD, Vita-Salute San Raffaele University, Milan, Italy
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Twitter: @zklaassen_md at the 2020 Genitourinary Cancers Symposium, ASCO GU #GU20, February 13-15, 2020, San Francisco, California
References:
1. Zelic, Renata, Hans Garmo, Daniela Zugna, Pär Stattin, Lorenzo Richiardi, Olof Akre, and Andreas Pettersson. "Predicting Prostate Cancer Death with Different Pretreatment Risk Stratification Tools: A Head-to-head Comparison in a Nationwide Cohort Study." European urology (2019).
2. Barzi, Afsaneh, Primo N. Lara Jr, Denice Tsao‐Wei, Dongyun Yang, Inderbir S. Gill, Siamak Daneshmand, Eric A. Klein et al. "Influence of the facility caseload on the subsequent survival of men with localized prostate cancer undergoing radical prostatectomy." Cancer 125, no. 21 (2019): 3853-3863.
3. Porpiglia, Francesco, Enrico Checcucci, Daniele Amparore, Matteo Manfredi, Federica Massa, Pietro Piazzolla, Diego Manfrin et al. "Three-dimensional elastic augmented-reality robot-assisted radical prostatectomy using hyperaccuracy three-dimensional reconstruction technology: a step further in the identification of capsular involvement." European urology 76, no. 4 (2019): 505-514.
4. Marconi, Lorenzo, Thomas Stonier, Rafael Tourinho-Barbosa, Caroline Moore, Hashim U. Ahmed, Xavier Cathelineau, Mark Emberton, Rafael Sanchez-Salas, and Paul Cathcart. "Robot-assisted radical prostatectomy after focal therapy: oncological, functional outcomes and predictors of recurrence." European urology 76, no. 1 (2019): 27-30.
5. Calais, Jeremie, Francesco Ceci, Matthias Eiber, Thomas A. Hope, Michael S. Hofman, Christoph Rischpler, Tore Bach-Gansmo et al. "18F-fluciclovine PET-CT and 68Ga-PSMA-11 PET-CT in patients with early biochemical recurrence after prostatectomy: a prospective, single-centre, single-arm, comparative imaging trial." The Lancet Oncology 20, no. 9 (2019): 1286-1294.
6. Hoffman, Karen E., David F. Penson, Zhiguo Zhao, Li-Ching Huang, Ralph Conwill, Aaron A. Laviana, Daniel D. Joyce et al. "Patient-Reported Outcomes Through 5 Years for Active Surveillance, Surgery, Brachytherapy, or External Beam Radiation With or Without Androgen Deprivation Therapy for Localized Prostate Cancer." JAMA 323, no. 2 (2020): 149-163.


