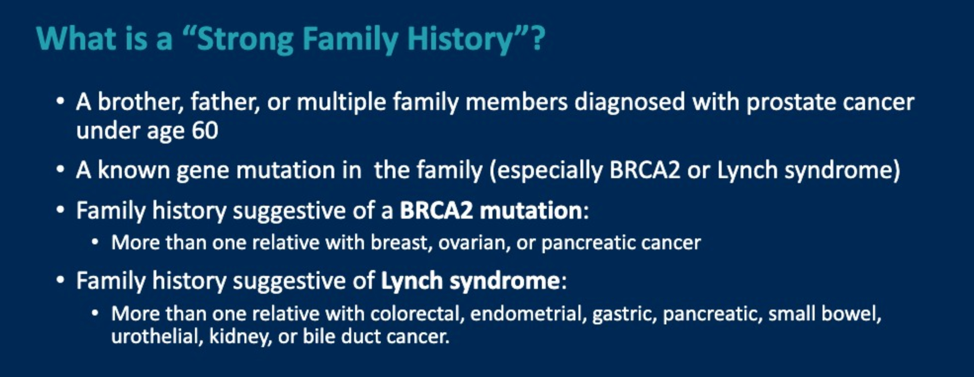
Before discussing the biopsy results, the panel raised the question of the family history and how it might change the approach to this case. The family history was felt to be strongly suggestive of BRCA2 germline alteration to the point that even if genetic testing was negative for commonly tested BRCA2 variants, the panel felt that other members in the family should have BRCA-focused genetic screening moving forward. The guidelines for genetic testing in prostate cancer were then reviewed.

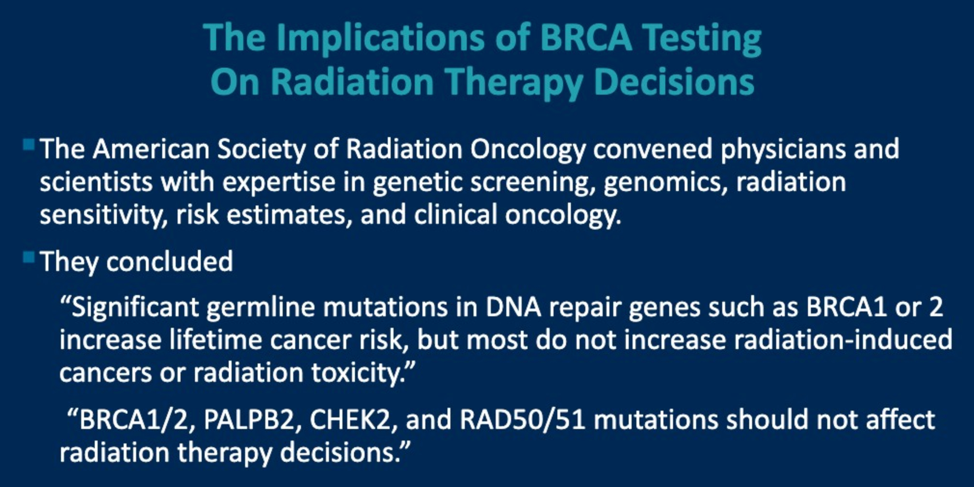
Additionally, the question was raised about the risk of administering radiation therapy to patients with DNA damage repair alterations such as BRCA. The short answer is these genomic changes should not impact the decision to administer radiation therapy.
Back to the case, the prostate biopsy showed Gleason 4+4 = 8 prostate cancer with extensive extraprostatic extension. A bone scan showed extensive metastatic disease. CT abdomen/pelvis showed no visceral involvement.
The question was raised about whether additional imaging would be helpful. The panel stated that Axumin® PET or PSMA PET would not change management in this patient and would not be additionally helpful. Some may consider an FDG-PET to get a sense of “aggressiveness”, but again, this would not change treatment decisions.
The patient went on to receive androgen deprivation therapy (ADT) along with six cycles of docetaxel chemotherapy with improvement in his urinary symptoms. Unfortunately, his PSA eventually started to rise and a tumor genomic test was sent.
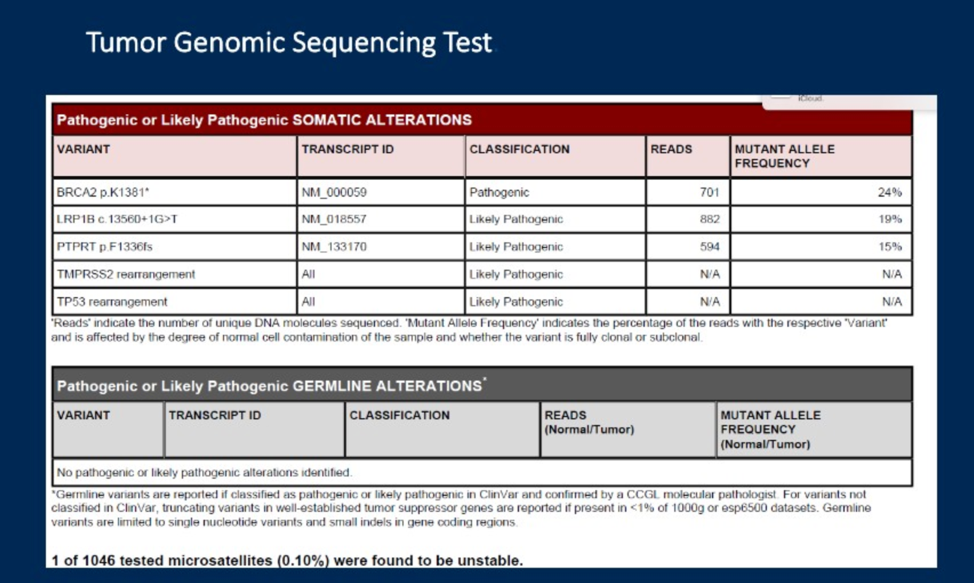
The impact of these genomic alterations on prognosis is complex given the alterations considered.
The patient’s PSA rose, and he was continued on observation until his PSA rose from 1.1 to eventually 11.4. Despite no metastatic lesions on conventional imaging, the patient wished to start therapy. He was started on abiraterone with a good response.
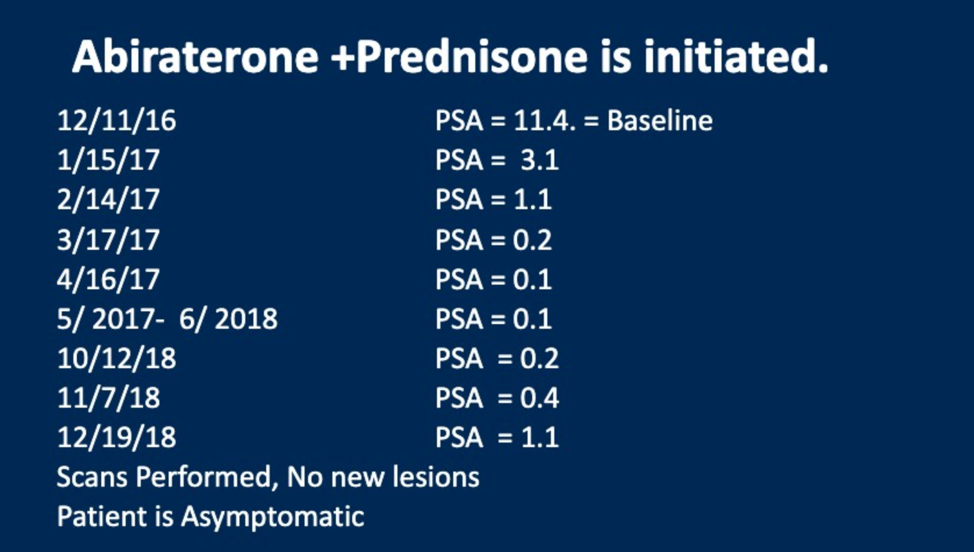
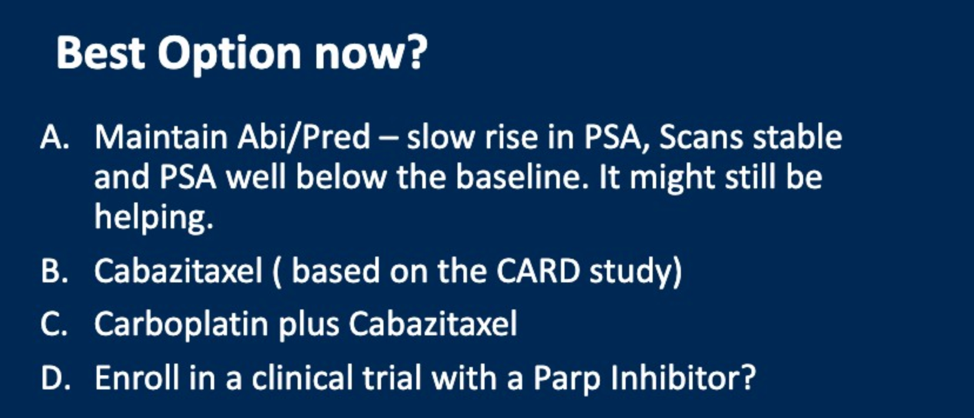
Based on the Phase III trials of abiraterone, treatment was not discontinued until there was a change in imaging findings. Therefore the patient was continued on abiraterone until there was imaging progression. Then based on his BRCA2 alteration, he was started on a poly (ADP-ribose) polymerase (PARP) inhibitor with the following response:
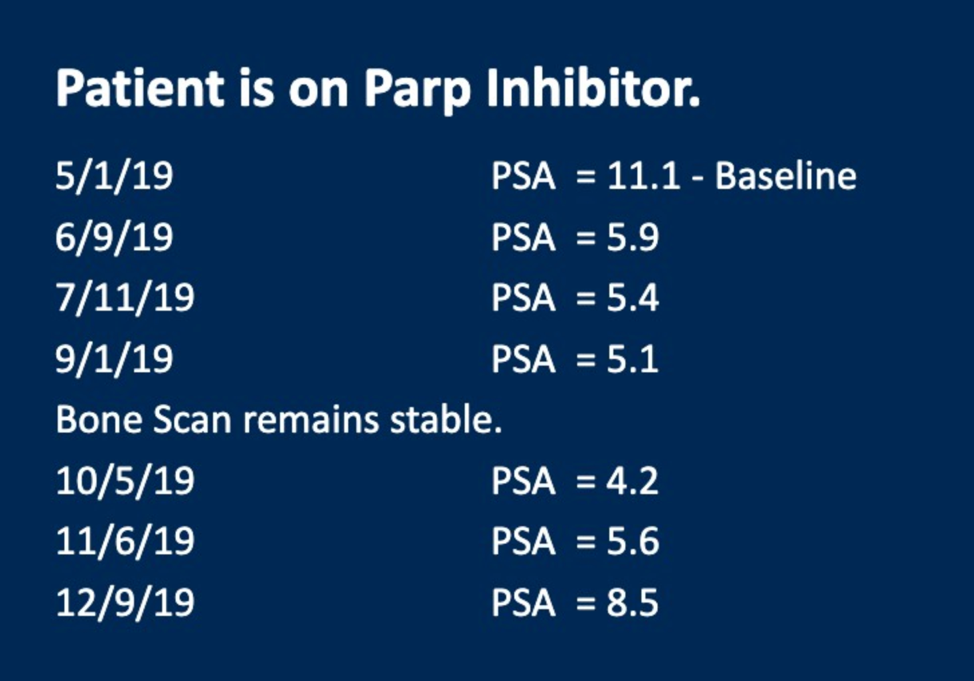
The final question was why was the PARP inhibitor not more effective. The reasons for this are unclear but could include a low mutant allele frequency, the presence of other genomic alterations that could abrogate response or differential response in patients with somatic versus germline alterations. The answer to this question will need further clinical and genomic follow-up over time as the prostate cancer community gains more experience with using PARP inhibitors to treat metastatic disease.
Presented by:
Charles J. Ryan, MD—Chair: B.J. Kennedy Chair in Clinical Medical Oncology at the University of Minnesota and Director of the Division of Hematology, Oncology and Transplantation.
Markus Graefen, MD—Chair: Professor of Urology & Chairman of Martini-Klinik, Prostate Cancer Center at the University Medical Center Hamburg-Eppendorf.
Scott Eggener, MD, Professor of Surgery and Radiology, Vice-Chair of Urology, Bruce and Beth White Family Professor of Urologic Oncology, Director, University of Chicago High Risk & Advanced Prostate Cancer Clinic (UCHAP), Chicago University, Chicago, Illinois
The Urologist Perspective
Karen Elizabeth Hoffman, M.D., M.H.Sc., M.P.H.
Department of Radiation Oncology, Division of Radiation Oncology, Associate Professor, Department of Radiation Oncology, Division of Radiation Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX
Radiation Oncologist
Celestia S. Higano, MD, FACP
Professor, Department of Medicine, Division of Oncology, Professor, Department of Urology, The University of Washington
Medical Oncologist
Thomas Hope, MD
Associate Professor, Radiology, School of Medicine, University of California, San Francisco
Radiologist
Written by: Alok Tewari, MD, PhD, Medical Oncology Fellow at the Dana-Farber Cancer Institute, Boston, Massachusetts at the 2020 Genitourinary Cancers Symposium, ASCO GU #GU20, February 13-15, 2020, San Francisco, California


