(UroToday.com) In recent years, significant improvements have advanced in the management of locally-advanced and metastatic urothelial carcinoma, including targeted small molecules, antibody-drug conjugates, and immune checkpoint inhibitors. Given these recent, and rapid, changes, the Dr. Gupta and colleagues sought to assess US physician treatment-decision and prescribing patterns using qualitative interviews (QIs) to approximate current real-world treatment trend data.

To establish a standard definition of recent studies, the authors started by evaluating relevant published abstracts in the field from January 2018 to March 2021, reflecting patients treated on study between 2000-2017. Following this, QIs were completed with 15 oncologists and urologists via 1:1 telephone interview of 1 hour in duration. All those interviewed were considered of adequate experience, namely in practice ≥1 year post fellowship, a board-certified oncologist/urologist, and managed ≥1 patient with locally-advanced or metastatic UC who received first-line (1L) systemic therapy in the past 6 months. QI respondents were community oncologists (n = 8), academic oncologists (n = 4), and community urologists (n = 3).
Summary of the published data revealed 40-65% of patients not receiving first-line systemic therapy. Among those patients receiving first-line treatment, a minority of patients went on to receive second-line therapy (range 15-40%). Of note, given the intrinsic latency between sharing of novel-drug treatment data, publication, and practice, the patient data collected was primarily prior to the close of 2017 so did not include the most recently established systemic therapies.
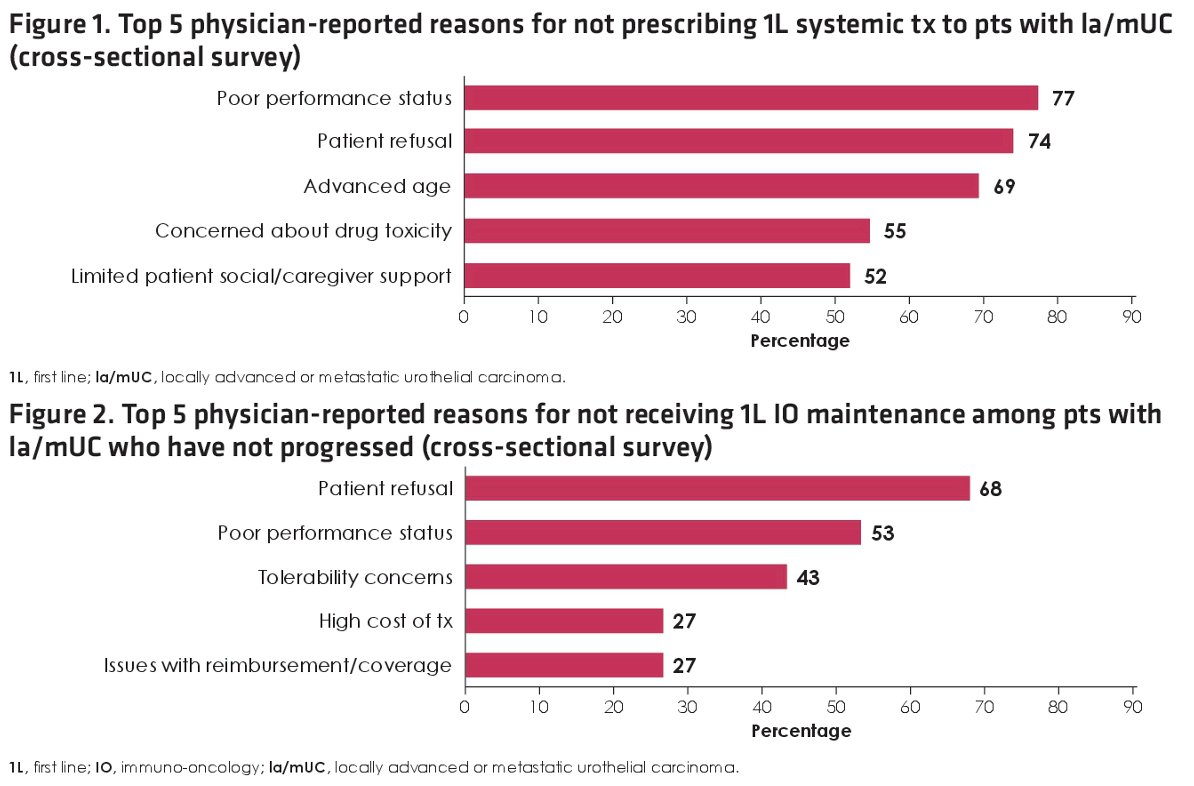
The average number was 23 patient of locally-advanced or metastatic UC patients among QI respondents. They estimated that greater than 75% of patients were currently receiving systemic therapy with all providing immunotherapy to eligible patients (10/11 were using avelumab). Increasing use of systemic therapy in recent years was noted in 11/15 (73%) of interviewees. Reported limitations to providing first line therapy included insufficient performance status (73%), advanced age (67%), patient preference (53%), and comorbidities (47%).
In those patients receiving first-line therapy, renal clearance, (100%) performance status (75%), extant neuropathy (75%), and age (50%) were considered as drug selection criteria.
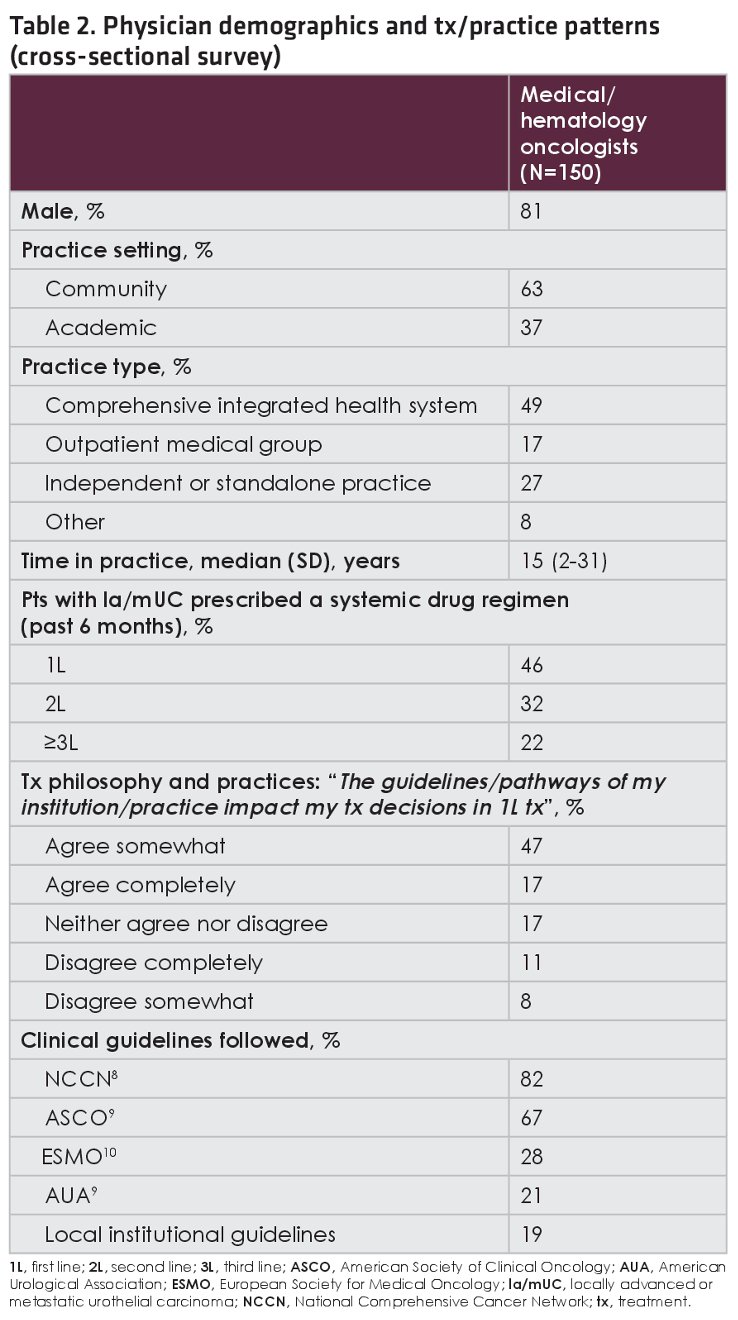
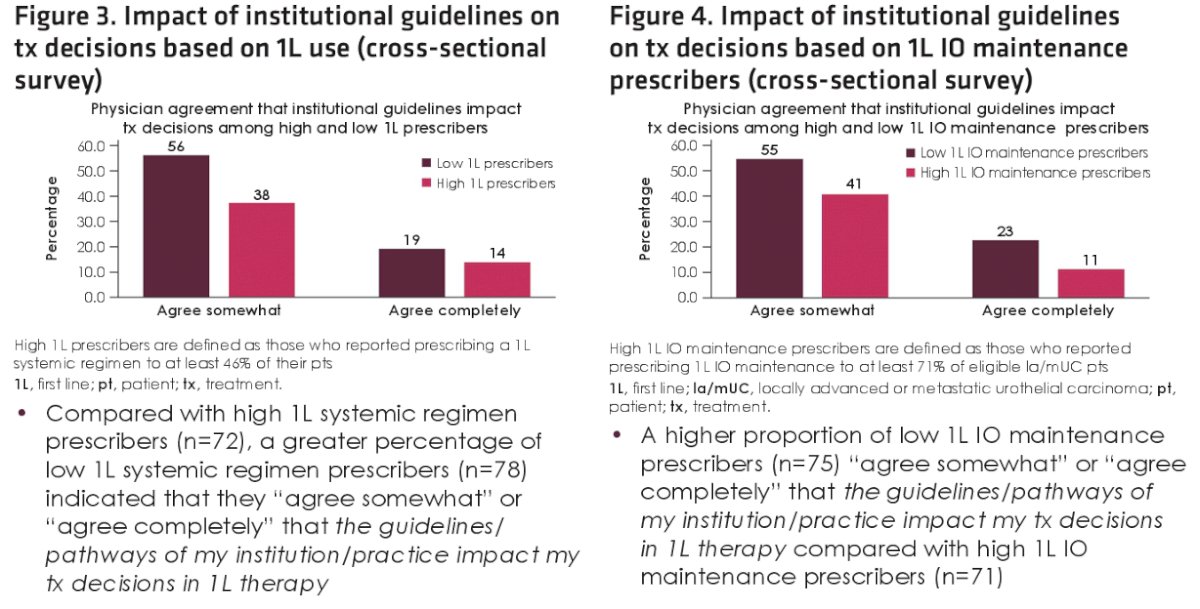
Perhaps to be interpreted as encouraging, the QI data suggested that current practice is more frequently providing systemic therapy to these patients. Among the trends include increasing use of systemic therapy including maintenance immunotherapy. Expansion to cross-sectional evaluation of 150 medical oncologists was included in the poster as expansion of this qualitative survey. In the larger data set (summarized in the Table 2 below), the authors were able to estimate the impact on institutional guidelines, stratified by high- or low-volume prescribers. These data, with limitations noted by the authors, is an relevant perspective on determining how available therapies and guidelines may result in treatment reaching patients in the first line for locally-advanced and metastatic bladder cancers.
Presented By: Shilpa Gupta MD, Taussig Cancer Institute, Cleveland Clinic Foundation, Cleveland, OH
Written By: Jones Nauseef, MD, PhD, Assistant Professor of Medicine within the Division of Hematology and Medical Oncology, Sandra and Edward Meyer Cancer Center, and Englander Institute for Precision Medicine at Weill Cornell Medicine and Assistant Attending physician at NewYork-Presbyterian Hospital. @DrJonesNauseef on Twitter during the 2022 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, Thursday Feb 17 – Saturday Feb 19, 2022


