(UroToday.com) The 2022 GU ASCO Annual meeting included a session on the management of rare variants in genitourinary cancers and a presentation by Dr. Karen Hoffman discussing the role of local therapy for prostate cancer variants. Dr. Hoffman notes that the prostate cancer histologic variants typically vary with regard to PSA production, frequency of metastasis at diagnosis, responsiveness to ADT, and their clinical course. As follows is a summary of survival outcomes stratified by histologic variant in the NCDB:

The prognosis of mucinous prostate cancer is similar to that of typical prostate adenocarcinoma and is defined by the presence of more than 25% extravasated mucin. This tumor produces PSA and does respond to androgen deprivation. Surgical series demonstrate favorable pathologic features and excellent cancer control for this histologic variant. Among 47 patients that underwent radical prostatectomy (mean PSA 9 ng/mL) at Johns Hopkins University, the mucinous component varied from 25% to 90%, with 13% Gleason 6, 78% Gleason score 7, and 9% Gleason 8 disease. The pathologic outcomes are highlighted in the following table:

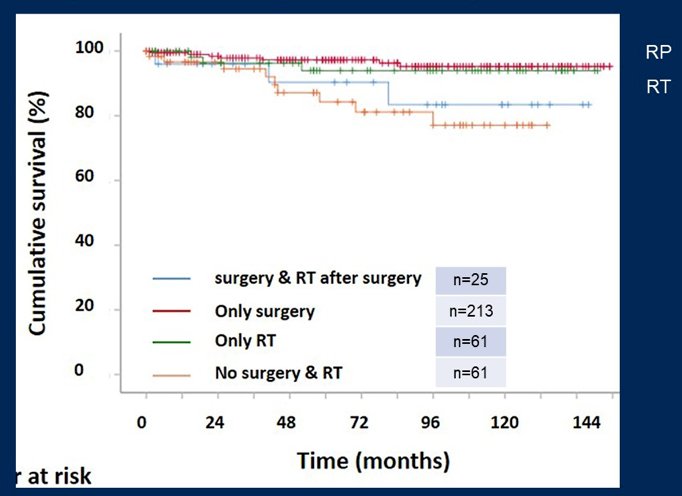
In this series, progression free survival at 5 years was 97%. At the population level, management of mucinous prostate cancer has been evaluated in the SEER database.1 In this series, 95-97% of patients were non-metastatic at diagnosis, and local therapy was curative for these patients. Prostatectomy was more frequently used (65%) than radiation therapy (24%), with the following stratified cancer-specific survival Kaplan-Meier curve:
Ductal adenocarcinoma is the most common histologic variant subtype of prostate cancer. Ductal adenocarcinoma can be challenging to diagnose, as PSA is unreliable, imaging can be misleading, and the disease is often diagnosed on TURP for obstructive symptoms. This subtype is more advanced at diagnosis as it is more likely to have T3 disease and lymph node involvement in prostatectomy series. In the NCDB and SEER database, approximately 12% of these patients are metastatic at diagnosis. Non-metastatic ductal prostate cancer is often approached like high-risk prostate adenocarcinoma, with higher failure rates noted than high-risk prostate adenocarcinoma. Prostatectomy usually includes lymph node dissection and nerves may need to be sacrificed, whereas radiation is usually delivered with ADT and dose-escalation with integrated or brachytherapy boost. As follows are metastasis-free survival curves stratified by ductal vs adenocarcinoma for those undergoing radical prostatectomy and radiotherapy:2

Dr. Hoffman notes that perhaps a multimodal approach is the best option for men with ductal prostate cancer, including prostatectomy followed by post-operative radiation with ADT. Surveillance after treatment should include imaging, since recurrence may not make PSA. Additionally, a chest CT should be considered given the risk of visceral metastasis. Prostate-directed radiation may be considered in the setting of metastatic ductal adenocarcinoma in order to reduce the tumor bulk, which may make systemic therapy more effective and prevent local symptoms and progression. In a series from the MD Anderson Cancer Center, 10% of patients with ductal variant and de novo metastasis responded to systemic therapy and underwent treatment of the primary tumor.
Small cell prostate cancer has an aggressive disease course with distinct morphologic features, high growth fraction, resistance to ADT, and short response to chemotherapy. Many patients are metastatic at diagnosis (63-77%), with dismal outcomes for these patients (median survival of 10 months):

Local therapy may benefit a select group of men with primary small cell carcinoma. A retrospective series of men with metastatic primary small cell carcinoma suggested that local therapy may improve outcomes and decrease morbidity from local pelvic symptoms:

The rarest of the rare histologic variants include adenosquamous (0.002%), sarcomatoid (0.003%), and signet ring (0.02%), as highlighted in the NCDB.

For these very rare variants, considerations for local treatment should consider if the tumor is localized or metastatic, assess whether the tumor is expected to cause local symptoms, and assess the anticipated clinical course.
Dr. Hoffman concluded her presentation of the role of local therapy for prostate cancer variants with the following take-home messages:
- Local therapy is usually appropriate for patient with localized disease, however cancer control outcomes vary across variants
- Local therapy can be considered for patients with metastatic disease in order to prevent morbid local symptoms and potentially improve outcomes
- Toxicity of treatment needs to be weighed against expected clinical benefit
Presented by: Karen E. Hoffman, MD, MHSc, MPH, Professor of Radiation Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, Thursday Feb 17 – Saturday Feb 19, 2022
References:
- Zhao F, Ziaokai Y, Xu M, et al. Mucinous prostate cancer shows similar prognosis to typical prostate acinar carcinoma: A large population-based and propensity score-matched study. Front Oncol. 2019;9:1467.
- Ranasinghe W, Shapiro DD, Hwang H, et al. Ductal prostate cancers demonstrate poor outcomes with conventional therapies. Eur Urol 2021;79(2):298-306.


