(UroToday.com) The 2022 GU ASCO Annual meeting included a prostate cancer session featuring work from Dr. Frank Schumacher and colleagues presenting results assessing the association of functional outcomes by decision-making approach in men with metastatic prostate cancer.
Multiple treatments with similar efficacy exist for metastatic prostate cancer resulting in multifaceted treatment choices. Shared decision-making engages patients and may be associated with superior outcomes in men with prostate cancer. Dr. Schumacher and investigators assessed the association of decision locus of control (shared decision-making vs. physician- or patient-directed decisions) and measures of patient quality of life, including patient reported functional outcomes and decision satisfaction.
Patients completed surveys of decision-making practices after a clinic visit in which a decision occurred. Patients also completed the EORTC QLQ-C30 quality of life instrument at baseline (time of decision), and 2- and 4-months. Scores for each quality of life dimension and pain were calculated for each time point, and the least-squared means were compared among decision locus of control groups to evaluate for associations using a mixed effects model.
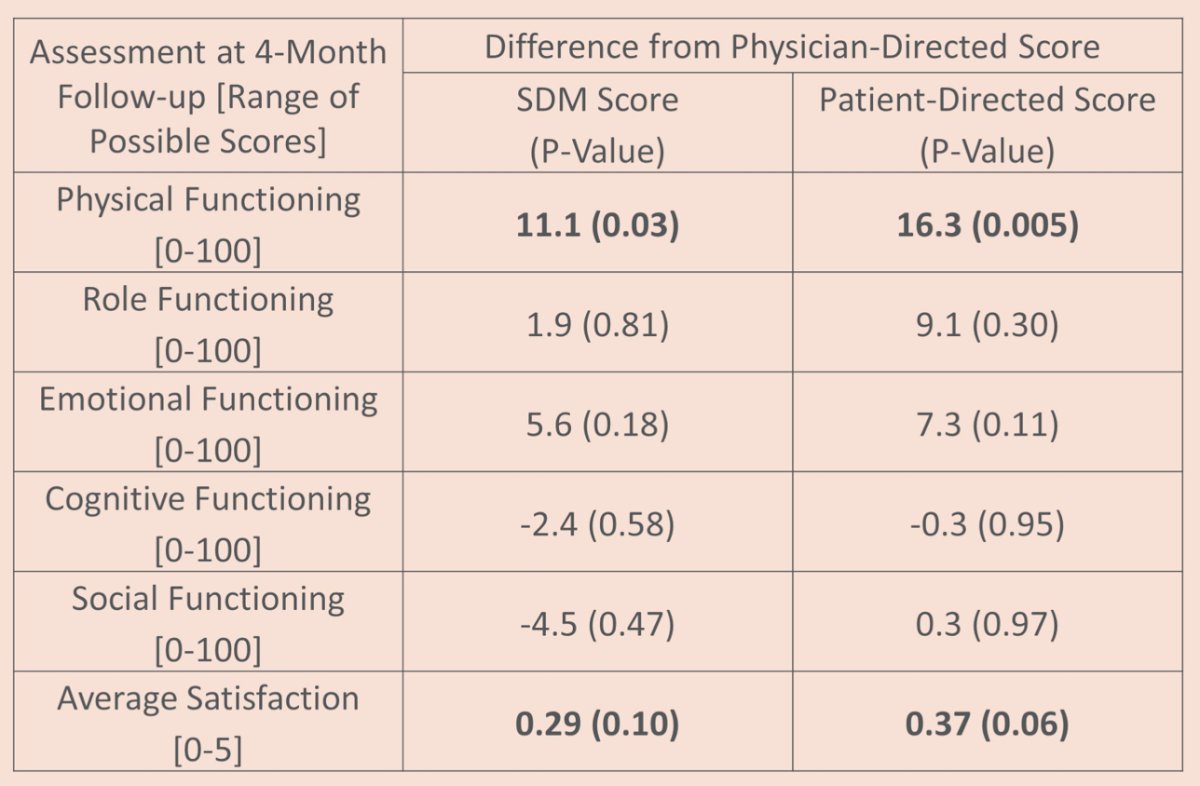
There were 101 patients that participated, with a median age of 69 years [range: 49-92], most patients were white (80%) and married (82%). A majority of patients reported experiencing shared decision-making in the clinic visit assessed (n = 63, 62%). At baseline, there was no significant difference in patient reported quality of life dimensions among decision locus of control groups, but patients reporting physician-directed decisions reported significantly greater baseline pain than the shared decision-making group. At 4 months, patient reported physical functioning was superior among patients reporting patient-directed (p=0.005) or shared decision-making (p=0.03) than those who reported physician-directed decision-making. There was a trend toward greater decision satisfaction among patients who reported patient-directed (p=0.06) or shared decision-making (p=0.10) at 4-months compared to men reporting physician-directed decision-making. There were no differences at 4 months for social, emotional, cognitive, or role functioning between decision locus of control groups:
Several potential limitations of the current study include (i) recall bias given the reliance on patient reporting, and (ii) the population was mostly white, married, and insured patients, thus limiting heterogeneity.
Dr. Schumacher concluded his presentation assessing the association of functional outcomes by decision-making approach in men with metastatic prostate cancer with the following take-home messages:
- Patients who reported greater control during treatment decisions had superior physical functioning and a trend toward greater decision satisfaction at 4 months compared with patients reporting physician-directed decisions, suggesting measurable domains of benefit from involvement in the decision-making process
- Continued research evaluating the association between physical and psychological outcomes and decision locus of control is needed, including larger studies within more diverse populations
Presented by: Frank Schumacher, MD, Northwestern University Feinberg School of Medicine, Chicago, IL, Northwestern University Department of Preventive Medicine, Chicago, IL
Co-Authors: Irene B. Helenowski, Kelvin A. Moses, James Benning, Alicia K. Morgans
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, Thursday, Feb 17 – Saturday, Feb 19, 2022


