Dr. Kool began his presentation by noting that the current paradigm for muscle-invasive bladder cancer management includes either a radical cystectomy with a pelvic lymph node dissection or radiation-based therapy, commonly in the form of tri-modality therapy. The rational for PLND with RC is the incidence of micrometastatic nodal occult disease in up to 40% of patients.1 Furthermore, PLND in this setting may be curative in a select cohort of patients. As such, there may be a similar rationale to widening radiotherapy fields to include pelvic lymph nodes as well, to improve oncologic benefits, particularly in high-risk patients.
As such, the objective of this study was to evaluate response to radiotherapy and survival outcomes in patients undergoing bladder-only versus whole-pelvis radiation. The authors utilized a Canadian multicenter database that included patients with MIBC (cT2-4a N0-2 M0) from 2001 to 2018 at 10 academic centers who underwent radiation-based therapy with curative intent, defined as a dose ≥44 Gy. The authors conducted inverse probability of treatment weighting (IPTW) analysis to account for baseline patient differences, and further accounted for potential known confounders using regression multivariable analysis.
This database included a total of 864 patients, of whom 599 without missing data were included in the IPTW analysis. The median follow-up was 34 months. When assessing differences in baseline clinical characteristics between the two unadjusted treatment cohorts, patients in the whole pelvis XRT group had higher risk disease, whereby they were more likely to have cN1-2 disease (12.5 versus 2.2%), LV invasion (26.3% versus 16.1%), and receive NAC (20.9% versus 10.4%) and concurrent chemo (76.7% versus 56.5%).
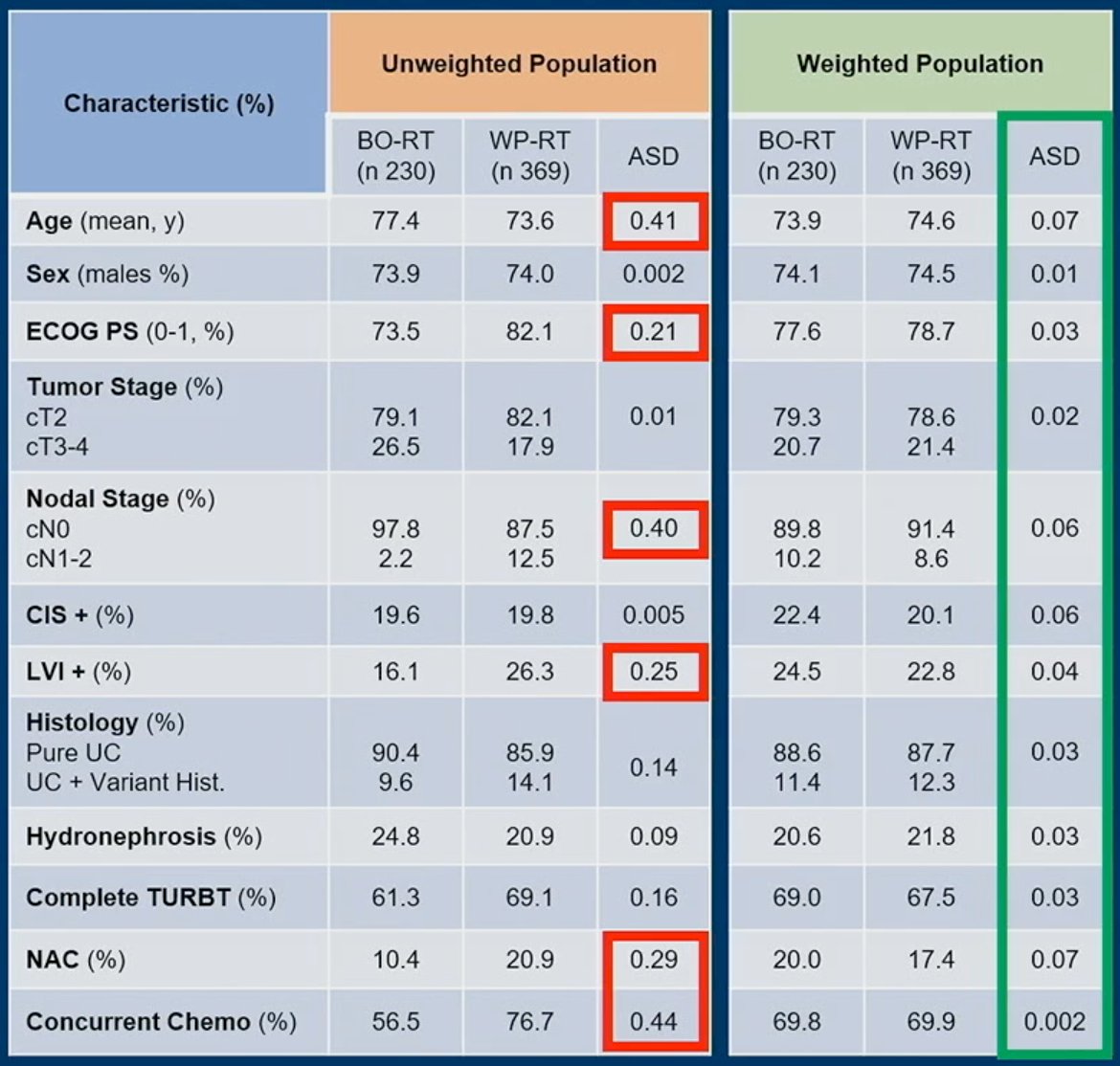
Following IPTW adjustment, these differences were no longer significant, as noted above.
As demonstrated in the KM curves below, cancer-specific and overall survivals were significantly improved in the whole-pelvis arm:
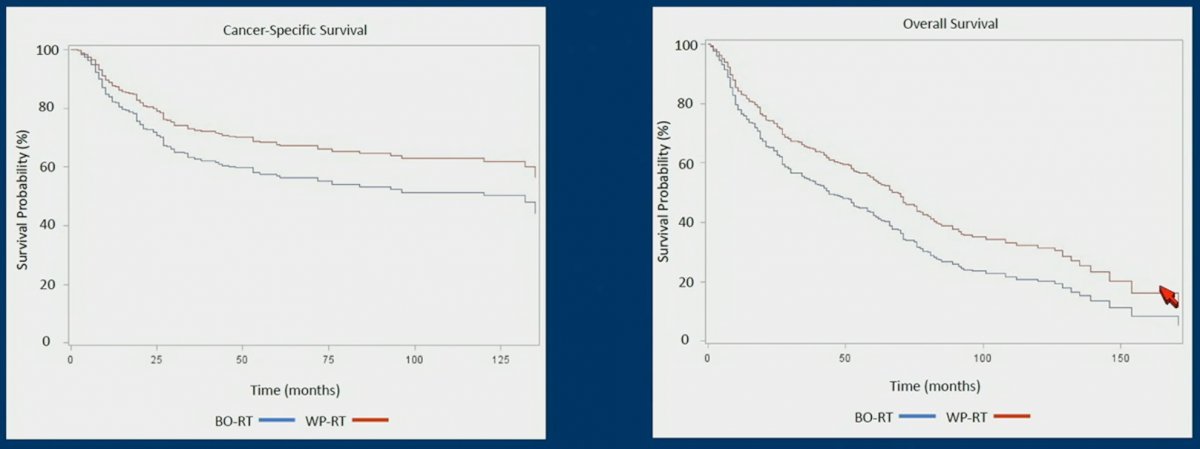
Following IPTW adjustment, a multivariable cox regression analysis evaluating the association of radiation volume with both CSS and OS, demonstrated that whole pelvis radiation was associated with significantly lower hazards of CSS (HR: 0.66, 95% CI: 0.47 – 0.93, p=0.016) and OS (HR: 0.68, 95% CI: 0.54 – 0.87, p=0.002).
With regards to complete response to radiotherapy, 127 had residual/persistent disease. On multivariable logistic regression analysis, receipt of whole pelvis XRT was not significantly associated with complete response odds (OR: 1.14, 95% CI: 0.76 – 1.72, p=0.53).
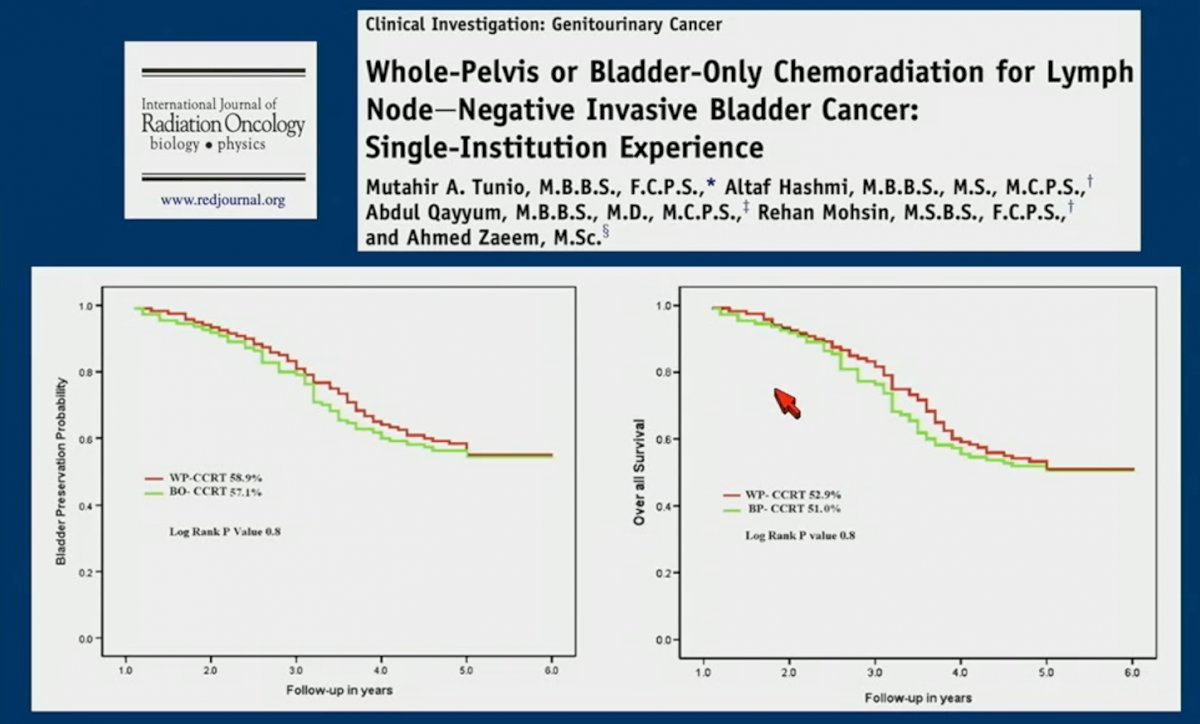
Dr. Kool pointed out that these results are in contrast to those reported by Tunio et al. which did not demonstrate significant differences in OS between patients receiving whole pelvis or bladder only radiotherapy. He did point out that patients in this study by Tunio et al. who received bladder only radiotherapy, did so with a 2 cm margin. As such, a significant portion of these patients also likely had their pelvic lymph nodes irradiated as well. With regards to grade 3-4 acute toxicity in the study by Tunio et al., this was observed in 17.6% and 13.3% of patients in the whole pelvis and bladder-only groups, respectively (p=0.05).2
Dr. Kool acknowledged that limitations to this study include its retrospective design with various treatment protocols, use of IPTW which accounts for known imbalances only, and that toxicity was not evaluated in this cohort.
Dr. Kool concluded that whole pelvis radiation might be associated with improved survival with prospective validation needed.
Presented by: Ronald Kool, MD, PhD Candidate at McGill University, Urologic Oncologist at Erasto Gaertner Hospital, Curitiba, Brazil
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, San Francisco, CA, February 16th – February 18th, 2023
References:- Madersbacher S, et al. Radical cystectomy for bladder cancer today--a homogeneous series without neoadjuvant therapy. J Clin Oncol 2003;21(4):690-6.
- Tunio MA, et al. Whole-pelvis or bladder-only chemoradiation for lymph node-negative invasive bladder cancer: single-institution experience. Int J Radiat Oncol Biol Phys 2012;82(3):e457-62.


