(UroToday.com) On the second day of the American Society for Clinical Oncology (ASCO) Genitourinary Cancer Symposium 2023 focussing on urothelial cancer, the Poster Session B: Prostate Cancer and Urothelial Carcinoma included a presentation from Dr. Scott Tagawa with updated outcomes from cohort 1 of TROPHY-U-01, assessing sacituzumab govitecan (SG) in patients with metastatic urothelial cancer (mUC) who had previously received platinum-based chemotherapy and a checkpoint inhibitor (CPI).
Sacituzumab govitecan is an antibody-drug conjugate composed of an anti-Trop-2 antibody coupled to SN-38, a topoisomerase-I inhibitor, via a proprietary hydrolyzable linker. On the basis of the primary analysis of the TROPHY-U-01 Cohort 1 study, sacituzumab govitecan received accelerated FDA approval in April 2021 in patients with mUC who previously received PT-based therapy and a CPI. As of that report, with a 9.1 month median follow-up, sacituzumab govitecan monotherapy demonstrated a 27% objective response rate (ORR) and median overall survival (OS) of 10.9 months among 113 patients with locally advanced or mUC progressing after receiving at least a PT-based therapy and a CPI. In this abstract, the authors provide updated outcomes for this cohort with extended follow-up.
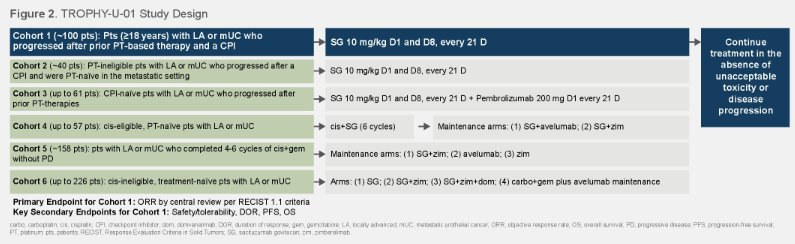
As previously described, TROPHY-U-01 (NCT03547973) is a multicohort, open-label, phase 2 study. Cohort 1 of this trial, included adult patients (age 18 years or older) had progression of mUC following PT (as first-line metastatic therapy or as (neo)adjuvant therapy with recurrence/progression ≤12 months) and CPI. Additionally, patients had to have ECOG PS 0-1 and creatinine clearance ≥30 mL/min. Following enrollment, patients received 10 mg/kg of sacituzumab govitecan intravenously on D1 and D8 of 21-D cycles. The primary endpoint was ORR per central review by RECIST 1.1. Key secondary endpoints included duration of response (DOR), progression-free survival (PFS), clinical benefit rate (CBR), OS, and safety.
As previously reported, the study cohort comprised 78% men with a median age of 66 years of whom 66% had visceral metastases (34% liver). Included patients were heavily pretreated with a median of 3 prior therapies (range, 1-8) and the median time since last prior therapy of 1.5 months (range, 0-60.0).
As of a data cut off on July 26, 2022, the median follow-up was 10.5 months (range, 0.3-40.9). According to central review, the ORR was 28% (95% CI, 20.2-37.6), consistent with the primary analysis. Additionally, assessing secondary endpoints, the CBR was 38% (95% CI, 29.1-47.7), the median DOR was 6.1 months (95% CI, 4.7-9.7, n=32) and the median PFS was 5.4 months (95% CI, 3.5-6.9).
Further, the median time to response was 1.6 months (range, 1.2-5.6) and median OS was 10.9 months (95% CI, 8.9-13.8).
Landmark DOR, PFS, and OS rates (95% CI) at 12 months were 30% (13.6-48.8), 14% (7.2-23.3), and 45% (35.4-53.8), respectively, with 7 (6%) patients still receiving sacituzumab govitecan at 12 months. Among those patients who received prior enfortumab vedotin (n=10) and prior PT in the (neo)adjuvant setting (n=39), results were consistent with the overall population.
Grade ≥3 treatment-related adverse events (TRAEs) occurred in 65% of patients and were similar to prior reports with the most common Grade 3 or greater TRAEs comprising neutropenia (35%), leukopenia (18%), anemia (14%), diarrhea (10%), and febrile neutropenia (10%). One treatment-related death occurred due to febrile neutropenia-related sepsis.
Thus, Dr. Tagawa concluded that this extended follow-up on TROPHY-U-01 with 10.5 months median follow-up demonstrates ongoing evidence of a high response rate to sacituzumab govitecan in patients with heavily pretreated mUC, including those with visceral metastases, prior EV therapy, and prior (neo)adjuvant PT therapy.
Presented by: Scott T. Tagawa, MD, MS, FACP | Weill Cornell Medical College of Cornell University

