(UroToday.com) The 2023 GU ASCO annual meeting included a session on addressing challenges to ensure health equity in bladder cancer, featuring a presentation by Dr. Christine Ibilibor discussing eliminating differences in outcomes by race and gender in urothelial carcinoma. The objectives of Dr. Ibilibor’s talk were to (i) review differences in survival outcomes based on race and gender in urothelial carcinoma, (ii) discuss multi-level factors contributing to differences in oncologic outcomes, and (iii) propose a framework for mitigating racial and gender-based disparities.
Dr. Ibilibor started by highlighting that there are overall and cancer-specific survival differences based on gender. Work from Williams et al.1 looked at data from SEER-Medicare and found that using propensity score matching, women had worse overall (HR 1.07, CI: 1.01-1.14), and worse cancer-specific survival (HR 1.26, CI: 1.17-1.36) than men. In the upper tract urothelial carcinoma setting, data are limited, but there is a generally high cancer-specific mortality rate and women are more likely to have higher tumor stage at diagnosis. Dr. Ibilibor notes that currently there is conflicting overall survival data for upper tract disease.
With regards to race-based differences in overall survival in bladder cancer, recent work from the American Cancer Society suggests a decreased 5-year overall survival for Black/African American patients, with these men and women having higher tumor stage at diagnosis:
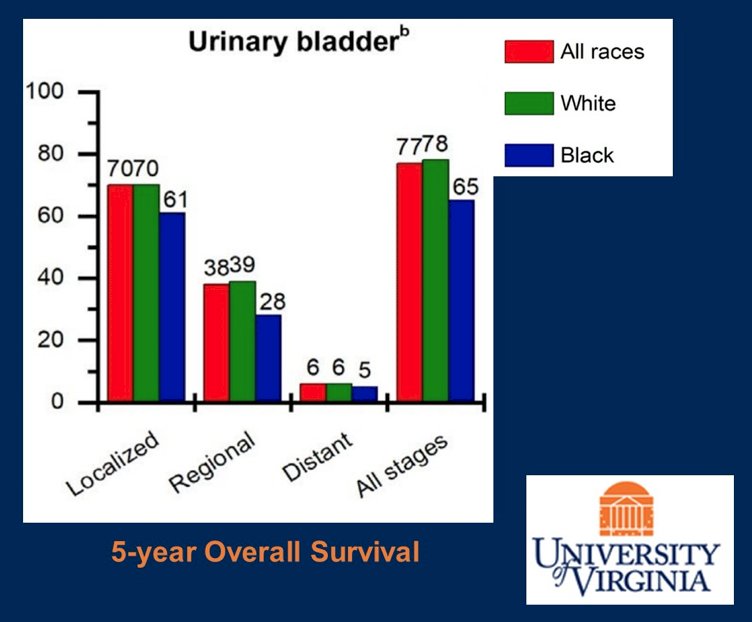
Again, in the upper tract urothelial carcinoma disease space, data is limited for assessing race-based differences, however Asian and Black/African American patients are more likely to have nodal involvement: 19.0% Asians, 17.1% African Americans, 15.0% Caucasians, 12.6% Hispanic (p < 0.001). Dr. Ibilibor emphasized that it is important to understand factors contributing to gender and race-based disparities in survival, which may be patient-related, provider-related, and system-related, all of which may lead to a delay in treatment:
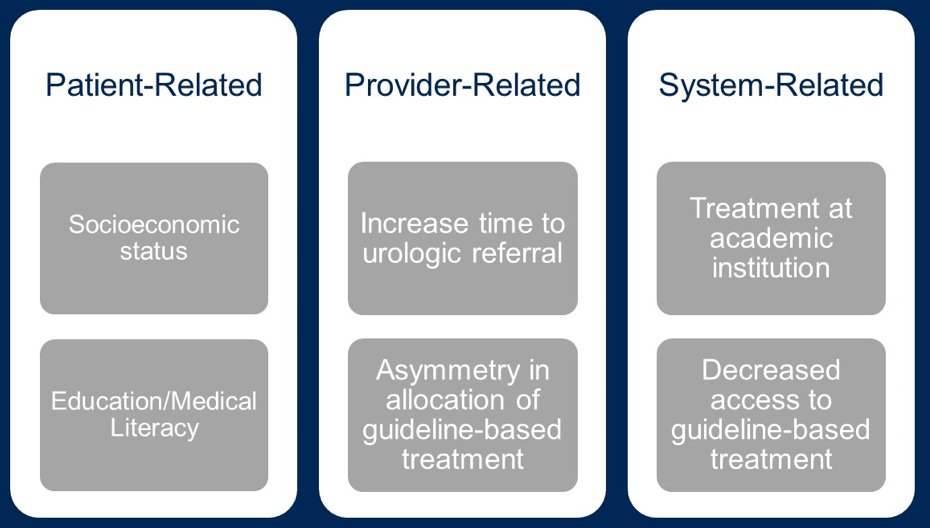
Patient related factors contributing to race-based disparities in survival are multifactorial. First, Black/African American and Hispanic patients with muscle invasive bladder cancer are more likely to experience treatment delay (OR 1.26 and 1.29, respectively). Second, lower education is associated with delay in time to treatment, given that 71% and 68% of Black/African American and Hispanic patients, respectively, live in zip codes with >=13% lacking a high school education. Provider related factors include women being more likely to have three or more visits with their primary physician prior to urologic evaluation for gross hematuria for bladder cancer compared to men.
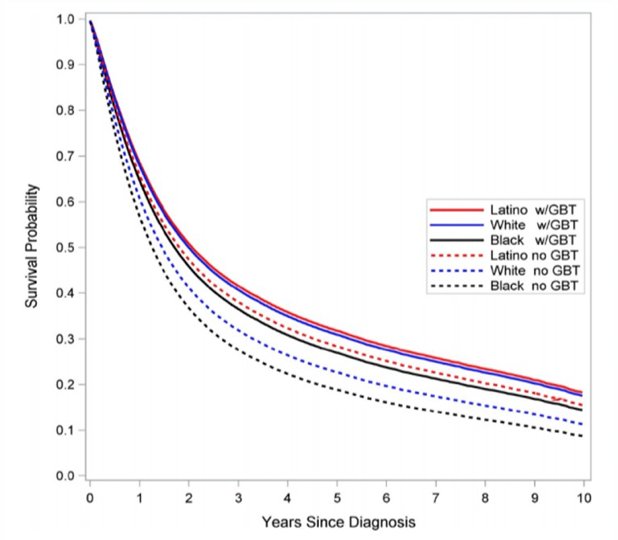
System related factors include treatment at an academic institution, associated with an OR of 1.22 for delay in treatment among 55% and 49% of Black/African American and Hispanic patients, respectively, with muscle invasive disease. Additionally, receipt of guideline-based treatment was only 45% for Black/African American and 48% for Latino patients among those with muscle invasive disease:2
Dr. Ibilibor provided the following framework for mitigating disparities:
- System-related factors: policy measures to improve access to guidelines-based treatment
- Provider-related factors: Decrease time to urologic evaluation, and increasing allocation of guideline-based treatment
- Patient related factors: enhance community outreach and education
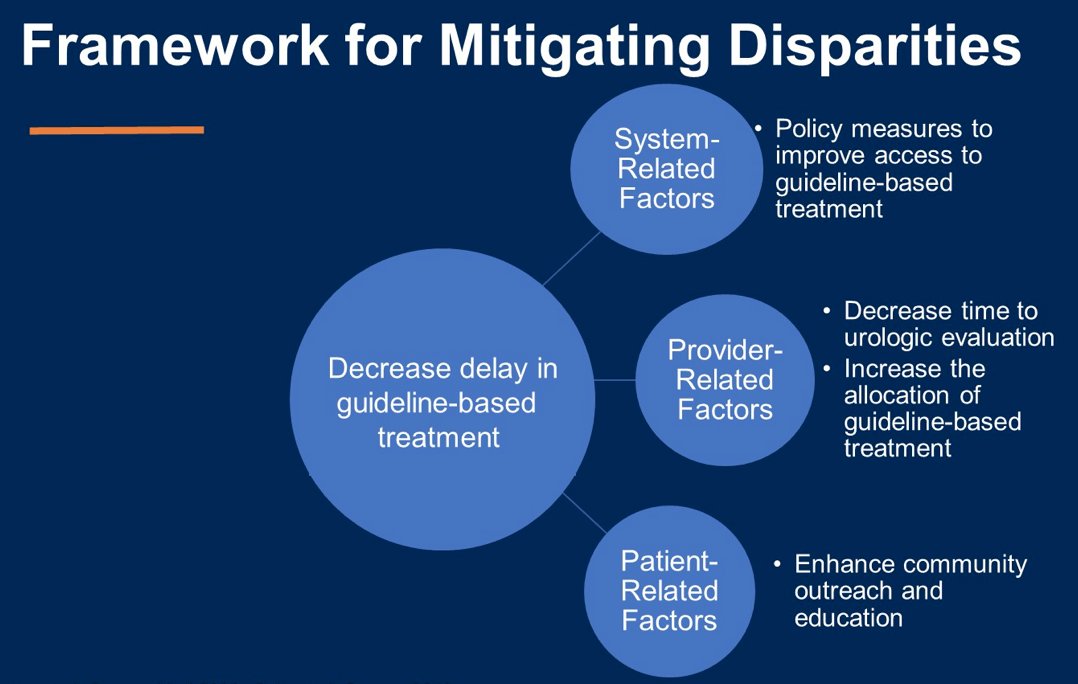
With respect to social determinants of health, it is important to understand that guideline-based treatment alone does not eliminate all the disparities in survival outcomes. Furthermore, inequities in social determinants of health can also account for these disparities, and system level interventions are key.
Dr. Ibilibor concluded her presentation discussing eliminating differences in outcomes by race and gender in urothelial carcinoma with the following concluding messages:
- Gender and race-based disparities are complex and no single intervention can remedy them
- However, delay in guideline-based care may lie at the core of some of these disparities
- Data related to interventions in this realm are limited, but consideration of these disparities with the context of social determinants of health and with multilevel approach is key for closing these gaps
Presented by: Christine Ibilibor, MD, University of Virginia, Charlottesville, VA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 Genitourinary (GU) American Society of Clinical Oncology (ASCO) Annual Meeting, San Francisco, Thurs, Feb 16 – Sat, Feb 18, 2023.
References:
- Williams SB, Huo J, Dafashy T, et al. Survival differences among patients with bladder cancer according to sex: Critical evaluation of radical cystectomy use and delay to treatment. Urol Oncol. 2017 Oct;35(10):602.
- Washington SL 3rd, Gregorich SE, Meng MV, et al. Race modifies survival benefit of guideline-based treatment: Implications for reducing disparities in muscle invasive bladder cancer. Cancer Med. 2020 Nov;9(22):8310-8317.


