(UroToday.com) The 2023 GU ASCO annual meeting included a session on addressing challenges to ensure health equity in bladder cancer, featuring a presentation by Dr. Vidit Sharma discussing the impact of the financial cost of bladder cancer. Dr. Sharma notes that bladder cancer is expensive, with SEER-Medicare 2015-2030 projections estimating that bladder cancer will cost $11.6 billion in 2030:

Cost is a matter of perspective, including patient, insurance/payer, and societal costs:
- For patients, this includes “direct” out of pocket costs and “indirect” costs, such as time off work, travel, and lodging
- For insurance/payers, this is the easiest to measure and study, with available government and private insurance data
- For society, this includes patient + payer costs and indirect societal costs, such as caregiver costs and reduced productivity
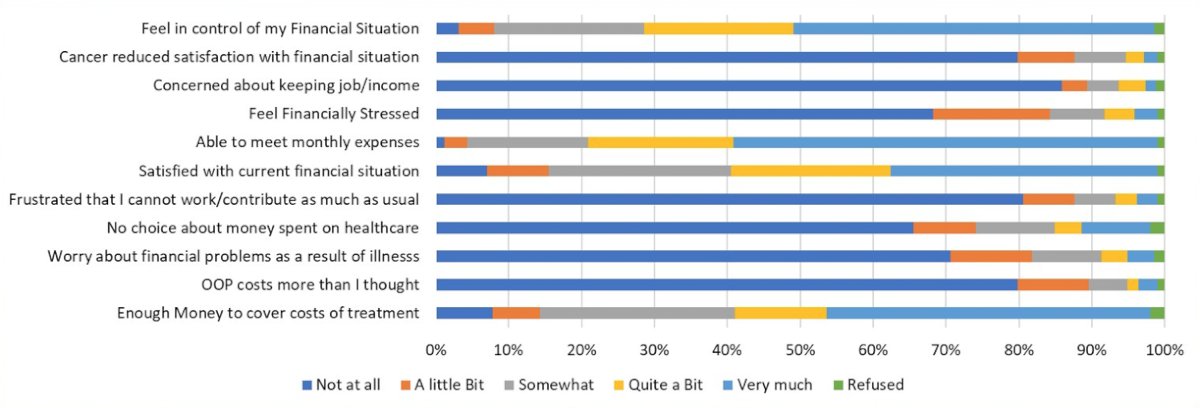
Direct costs are defined as dollars exchanged between hospitals/providers and patients (out of pocket costs) and insurers (payer costs). Indirect costs are defined as monetary costs not given to hospitals/providers, such as travel, meals, time off work, unpaid leave, and care-giver costs. In 2002, it was estimated that patients had >$2,000/year in time lost alone and ~$150,000 in lifetime indirect costs. The ramifications of patient costs are financial toxicity, via material (debt, reduced income, bankruptcy), psychological (worry, distress), and behavioral (skipping medications/visits), which may compromise treatment efficacy.
Dr. Sharma notes that there is significant financial toxicity in bladder cancer. In a survey of 144 patients from the UNC Bladder Cancer Cohort, 24% had financial toxicity “having to pay more for medical care than you can afford”.1 Financial toxicity was more common in younger, black, and patients without a college degree, and also correlated with lower quality of life scores.
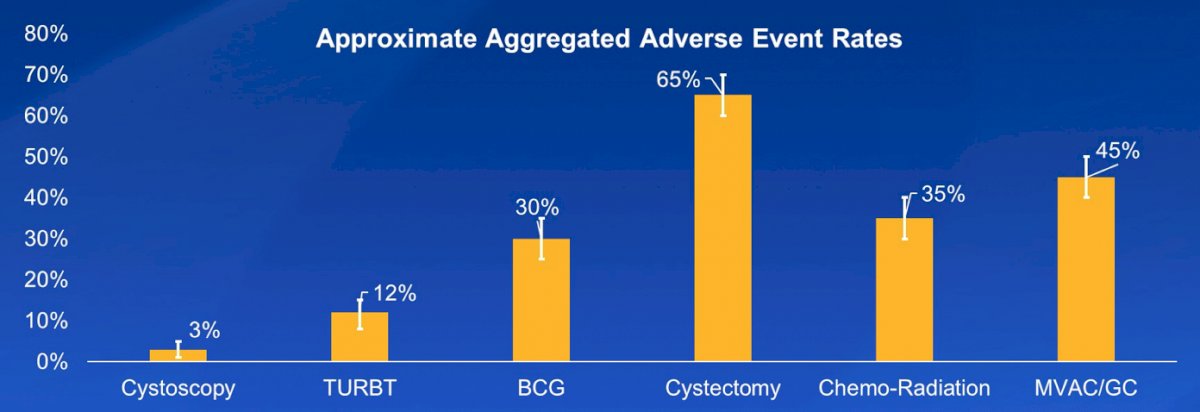
With regards to sources of costs of bladder cancer, complications increase costs significantly. In fact, 30% of direct Medicare costs (1991-1999) from bladder cancer were related to complications, thus preventing complications can reduce costs:
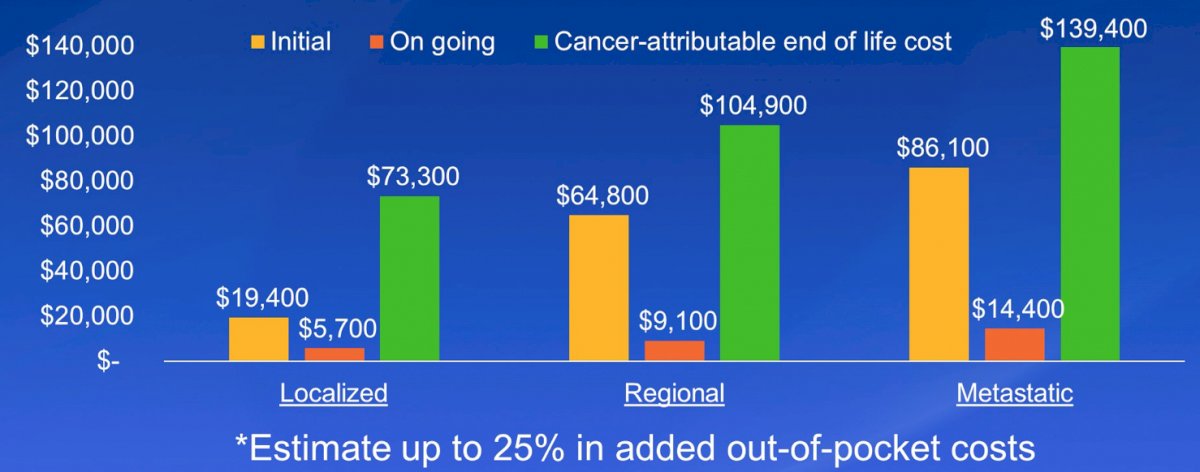
Additionally, Medicare costs increase by stage:
Dr. Sharma also noted that in patients with non-muscle invasive disease, costs increase by risk of progression, with progression to muscle invasive bladder cancer accounting for 70%-90% of total costs. Preventing progression is an important way to reduce the costs of NMIBC. Work from Dr. Sharma and colleagues looked at the Kaiser Permanente NMIBC cohort (412 patients with cost data), finding that 4-16% of participants reported some financial strain and 5% significant financial burden. Importantly, AUA NMIBC risk was not correlated with financial toxicity:
With regards to strategies to mitigate cost and financial toxicity, it is important to (i) understand the financial concerns to identify at risk patients, (ii) connect at risk patients with resources, such as social work and financial navigators before treatment starts, and (iii) include financial concerns in shared-decision making. Finally, Dr. Sharma and colleagues used a decision-analytic Markov model to compare pembrolizumab, salvage intravesical chemotherapy (with gemcitabine-docetaxel induction + monthly maintenance) and radical cystectomy for patients with BCG-unresponsive carcinoma in situ who are radical cystectomy candidates (index patient 1) or are unwilling/unable to undergo radical cystectomy (index patient 2). They found that at its current price, pembrolizumab is not cost-effective for BCG-unresponsive carcinoma in situ relative to radical cystectomy or salvage intravesical chemotherapy. Dr. Sharma notes that by quantifying the tradeoffs, this methodology helps him identify the patient for whom each treatment is an appropriate choice.
Dr. Sharma concluded his presentation discussing the impact of the financial cost of bladder cancer with the following concluding messages:
- Bladder cancer has costs we can measure, which are often just the tip of the iceberg
- Costs are related to surveillance, progression, and complications
- Financial toxicity seems more dependent on insurance, income, employment, and younger age
- We can mitigate cost and financial toxicity by:
- Understanding financial concerns of patients
- Connecting at risk patients with resources early
- Value-driven shared-decision making
Presented by: Vidit Sharma, MD, Mayo Clinic, Rochester, MN
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 Genitourinary (GU) American Society of Clinical Oncology (ASCO) Annual Meeting, San Francisco, Thurs, Feb 16 – Sat, Feb 18, 2023.
References:
- Casilla-Lennon MM, Choi SK, Deal AM, et al. Financial Toxicity among Patients with Bladder Cancer: Reasons for Delay in Care and Effect on Quality of Life. J Urol. 2018 May;199(5):1166-1173.


