(UroToday.com) In this abstract, Shah and colleagues explore selection bias and disparities in surgical health care delivery of radical nephrectomy in patients with renal cell carcinoma.
As with other malignancies, disparities in outcomes of renal cell carcinoma (RCC) exist with respect to survival outcomes between different ethnic, and socioeconomic groups. The authors aimed to evaluate disparities in delivery of surgical care between medically underserved (MU) and non-medically underserved (NMU) patients.
This was a single-center retrospective analysis of consecutive patients presenting with localized renal cortical neoplasms who underwent surgical excision [Radical (RN) or Partial Nephrectomy (PN)] at an academic tertiary-care referral center (UC San Diego). The cohort was divided into MU and NMU groups - though it was never clear how this distinction was made. Descriptive analyses were conducted for demographics and clinical disease characteristics, type of surgery, time to surgery, estimated blood loss, and 30-day total and major complications (Clavien-Dindo, ≥3). Cochran-Armitage trend analysis was conducted to evaluate for surgical trends, and logistic regression multivariable analyses (MVA) were conducted for type of surgery and major complications.
1418 patients were analyzed (MU n=334, NMU n=1084).
Demographics of the cohorts are displayed below:
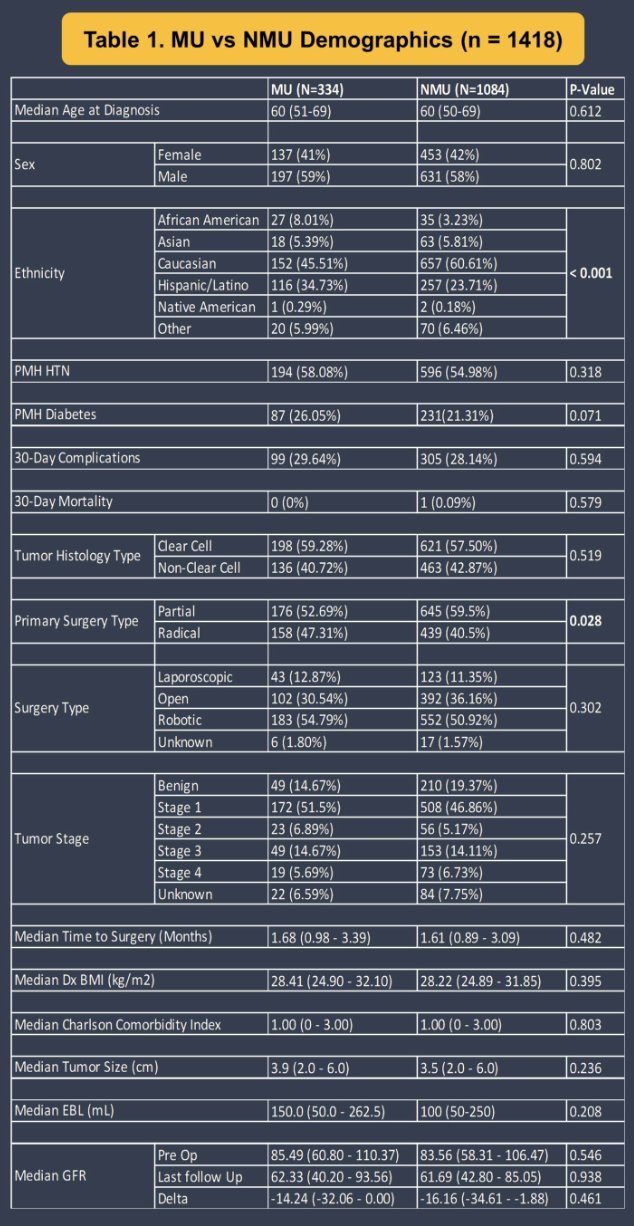
Comparing MU vs. NMU, no differences were noted for age (p=0.612), Charlson Comorbidity Index (p=0.803), tumor size (p=0.236), or time to surgery (p=0.482). Significantly greater proportions of white patients were noted in NMU (60.6% vs. MU=45.5%, p<0.001) and higher proportion of RN in MU (47% vs. NMU=40.4%, p=0.028).
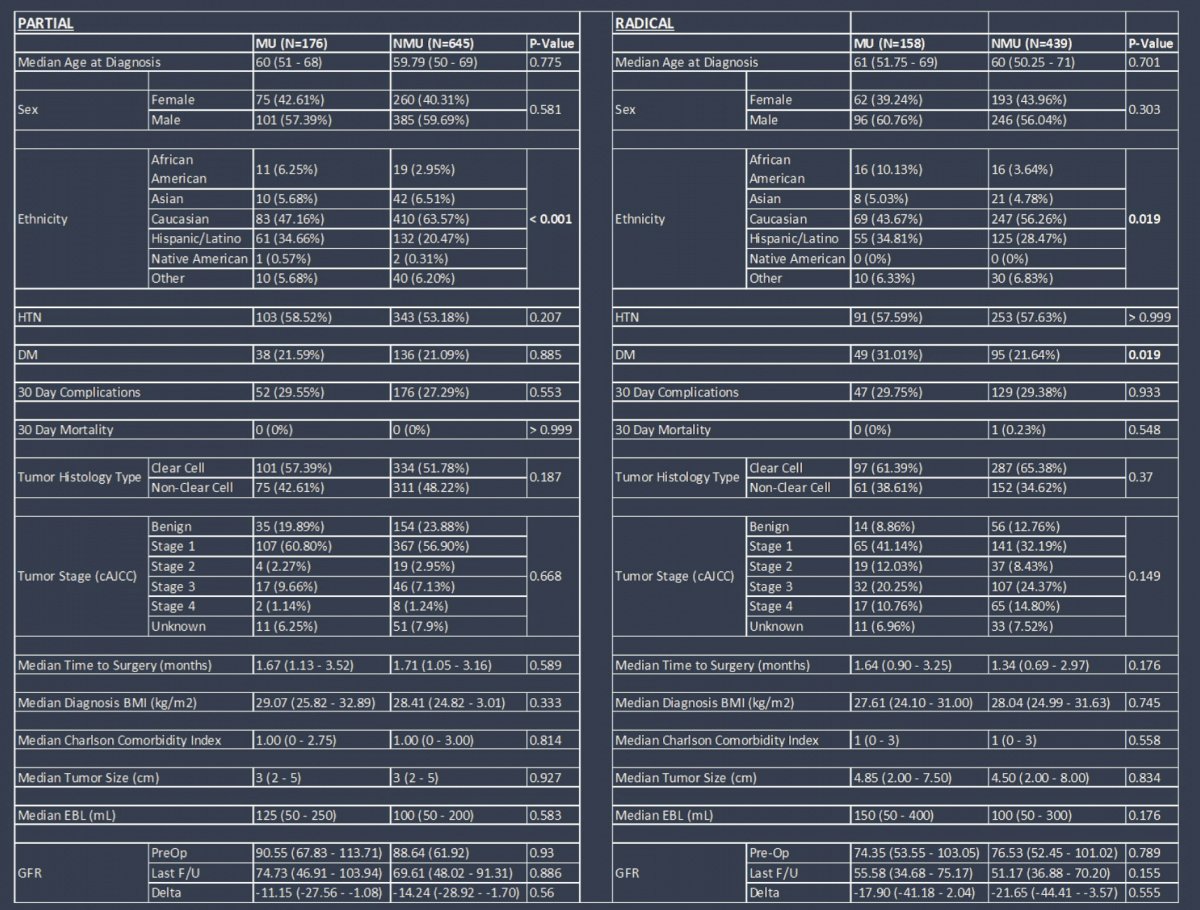
Subgroup analyses of PN groups revealed no differences with respect to demographics, tumor size (p=0.33), major complications (p=0.55), or blood loss (p=0.583). However, subgroup analysis of RN revealed significantly higher proportion of non-white patients (p=0.019) and patients with diabetes (p=0.019).
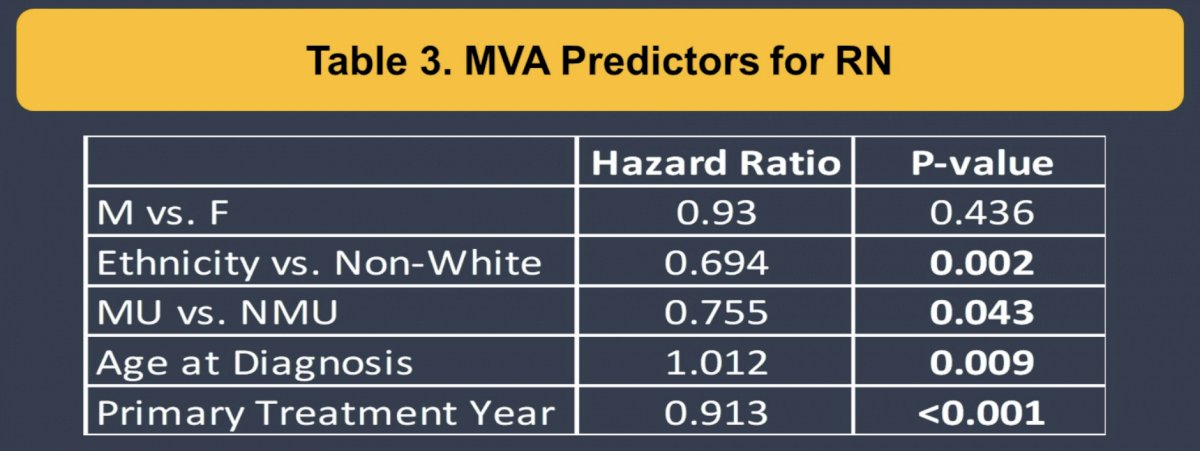
MVA: MVA for predictors for receipt of RN were non-white (OR1.4, p=0.002), MU (OR=1.32, p=0.043), age (OR=1.01, p=0.009) and treatment year (OR=0.913, p<0.001).
Cochran-Armitage trend analysis indicated that both MU and NMU had significant increases in PN between 2003 and 2021 (p<0.0001).
Based on this, the authors conclude that despite overall similarities with respect to demographics and clinical disease characteristics and time to surgery, MU status was associated with a significantly higher odds of receiving a RN at a tertiary care referral center, which represents a disparity in care and possible selection bias. Nonetheless, RN was also associated with a decreased risk of complications. While trends have demonstrated an increase in proportion of PN for both NMU and MU groups, comparative underutilization of PN in MU patients may be associated with increased downstream risks to health.
Presented by: Aastha Shah, BA | University of California San Diego, Department of Urology
Written by: Thenappan (Thenu) Chandrasekar, MD – Urologic Oncologist, Associate Professor of Urology, University of California, Davis @tchandra_uromd on Twitter during the 2023 Genitourinary (GU) American Society of Clinical Oncology (ASCO) Annual Meeting, San Francisco, Thurs, Feb 16 – Sat, Feb 18, 2023.


