(Urotoday.com) The first day of the American Society for Clinical Oncology (ASCO) Genitourinary Cancer Symposium 2023 began with four talks highlighting key data that, from the perspective of medical oncologists, urologic oncologists, radiation oncologists, and pathologists, advanced the needle in prostate cancer care in 2023.
Second among these talks was Dr. Christopher Wallis, presenting the key papers in prostate cancer from the urologic oncologist’s perspective. He began by noting that while the stereotypical surgeon’s question is one of a surgical approach, urologic oncologists contribute to the care of patients across the spectrum of prostate cancer from screening and diagnosis through the treatment of localized disease and recurrence to metastatic disease and even end of life care.
Considering this spectrum of care, the first key paper highlighted focused on population-level effects of prostate cancer screening. Dr. Wallis noted that for most patients in populations where screening is adopted, prostate cancer will be diagnosed in asymptomatic stages. Thus, we must weigh the benefits and harms of this early detection. He highlighted data published by Dr. Bryant and colleagues in JAMA Oncology which drew upon the rich data resources from the US Veterans Health Administration. These authors demonstrated, as others have done, that PSA screening rates and prostate biopsy rates have declined over the past decade. Not surprisingly then, rates of incidence prostate cancer have been falling. Importantly though, these authors demonstrated that while the incidence of non-metastatic prostate cancer decreased, the incidence of high-grade non-metastatic disease of metastatic prostate cancer have correspondingly increased.
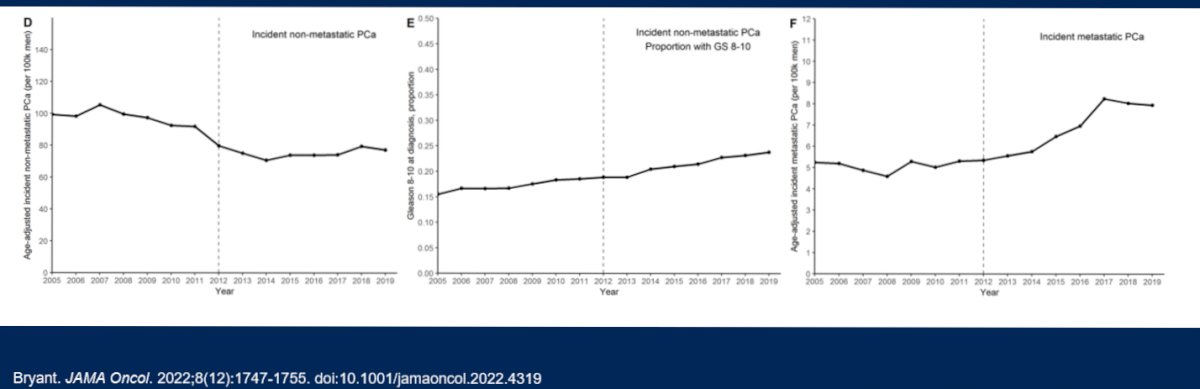
Taking these two observations together, rather than relying on inference, the authors assessed facility level utilization of PSA testing and subsequent rates of cancer diagnosis. As highlighted to the left of the figure below, as PSA screening rates increase, the subsequent number of metastatic prostate cancer cases fell. Conversely, as long-term PSA non-screening rates (defined as individuals with no PSA test in the preceding 3 years) increased, the number of metastatic prostate cancer cases increased.
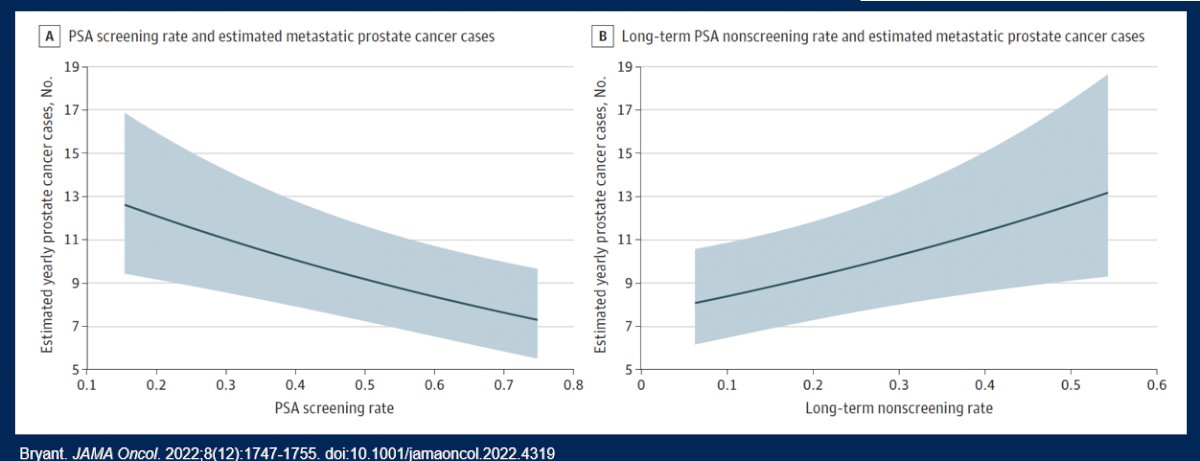
Dr. Wallis therefore highlighted that these data show us that while PSA screening rates have declined over time (across all age and racial subgroups), lower PSA screening rates are associated with higher subsequent diagnoses of metastatic prostate cancer.
Considering then how we screen and diagnose disease, Dr. Wallis moved to discussing the recently published GOTEBORG-2 trial. This study provided a randomized comparison of PSA screening followed by MRI with MRI-targeted biopsy. Importantly, this study showed that such an approach can significant decrease the diagnosis of clinically insignificant cancer without significantly affecting the diagnosis of clinically significant disease.

Thus, Dr. Wallis concluded that the GOTEBORG-2 trial has shown us that we can screen for prostate cancer in a way that reduces overdiagnosis and may of the down stream harms of prostate cancer screening, with only a modest increase in the risk of missing favourable intermediate risk disease.
However, he noted that there are a number of limitations with MRI including quality control issues at the level of both image acquisition and interpretation, the availability of scanners, and the time and cost associated. However, newer paradigms are assessing alternative approaches. One such approach that he highlighted is the use of bi-parametric, rather than multi-parametric, MRI. By sparing the contrast enhanced sequences as well as some of the orthogonal T2 sequences, bi-parametric MRIs are substantially quicker and less expensive. However, detection of clinically significant prostate cancer is relatively comparable between bi-parametric MRI (17% miss rate; NPV of 0.93) and multiparametric MRI (6% miss rate; NPV of 0.97), with misses being able to be captured based on either PSA density or use of mpMRI for patients with equivocal findings on bi-parametric MRI.
Applying these data to practice, Dr. Wallis presented the case of a 66 year old man who presented with an elevated PSA of 15.9 ng/mL and a left apical nodule on DRE. Notably, his PSA 9 months prior had been 2.1. Highlighting data from both the GOTEBORG-2 trial and the PRECISION study, this gentleman underwent a prostate MRI demonstrating a PI-RADS 5 lesion occupying essentially the entirety of the left side of the prostate cancer. The MRI further noted left sided neurovascular bundle invasion, extraprostatic extension, and seminal vesicle invasion, as well as multiple enlarged pelvic lymph nodes and enhancing bone metastases. Biopsy confirmed Grade Group 5 prostate cancer with both intraductal carcinoma and cribriform glands. Completion of his staging studies confirmed high-volume metastatic castration sensitive prostate cancer.
Dr. Wallis then noted, as discussed by Dr. Mehra, that 2022 provided new data supporting triplet treatment intensification with ADT, docetaxel, and a novel hormonal agent (abiraterone or darolutamide) for these patients. While noting some of the methodologic differences between the ARASENS and PEACE-1 trials, he emphasized that each of these have shown an overall survival benefit to the use of a triplet approach, compared to ADT and docetaxel.
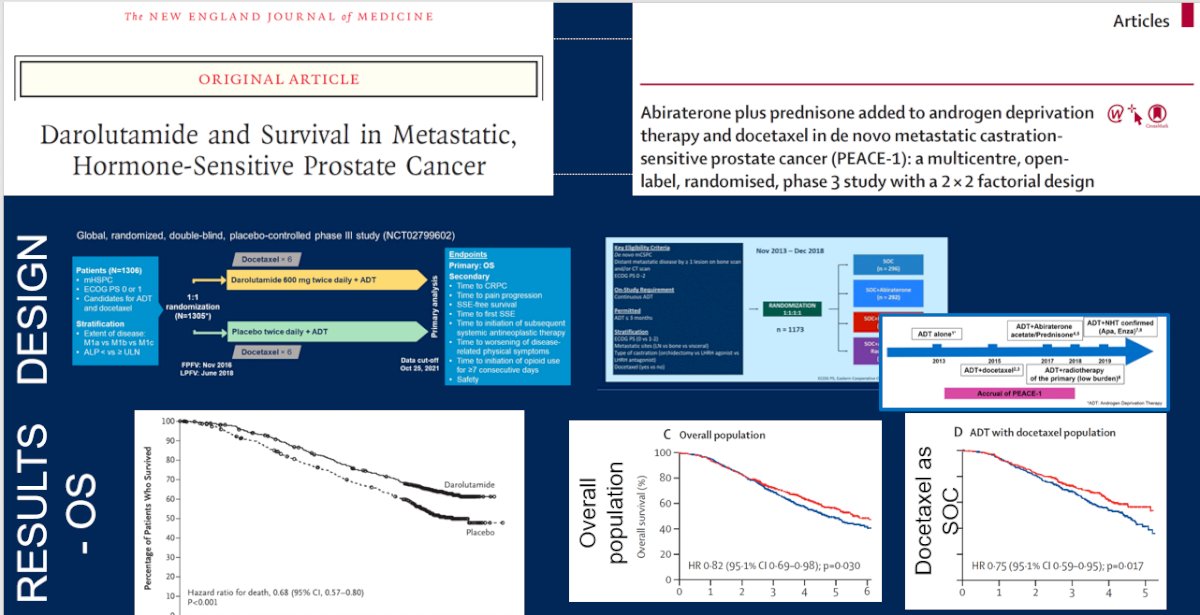
As we move these data to our clinics on Monday, he noted that the landscape of mCSPC treatment has changed in ways that are important for urologic oncologists. Prior to 2015, ADT monotherapy was the standard of care in this disease space and this was routinely given by urologists and radiation oncologists. Following publication of the CHAARTED data, docetaxel intensification become standard of care for many patients, necessitating referral to a medical oncologist. However, with the subsequent publication of data for novel hormonal agents, interested urologists could again take the lead on treating these patients with intensified regimes. Given the data for triplet therapy that has emerged over the past year, Dr. Wallis emphasized the importance of early involvement of medical oncologists in the care of these patients to ensure that all relevant treatment options are discussed.
Thus, in conclusion, he emphasized that the data from 2022 has shown us that appropriate prostate cancer screening can reduce the subsequent development of metastatic disease. Further, we can screen better, in a way that reduces the burdens and harms associated with overdiagnosis. Finally, patients with mCSPC deserve to meet with a medical oncologist to discuss triplet therapy before embarking on first-line treatment.


