(UroToday.com) On the first day of the American Society for Clinical Oncology (ASCO) Genitourinary Cancer Symposium 2023 focussing on prostate cancer, Dr. Stephen Freeland presented data examining racial differences in survival and healthcare resource utilization among Medicaid-insured adults with metastatic castration sensitive prostate cancer in Poster Session A.
It has been long recognized that there are racial disparities in American health care. Largely driven by these, Black or African American men have higher overall cancer death rates compared to other racial or ethnic groups. One of the disease sites with the greatest racial disparities is prostate cancer: prostate cancer incidence and mortality are both substantially higher among Black or African American men, though when matched for stage, whether outcomes differ by race is controversial.
In this study, the authors performed a retrospective longitudinal cohort study to assess for race-based differences in overall survival (OS) and healthcare resource utilization (HRU) among Medicaid-insured patients with metastatic castration-sensitive prostate cancer (mCSPC).
To do so, they used de-identified administrative claims data from the Centers for Medicare and Medicaid Services 100% Medicaid data files, from 01/01/2010 - 12/31/2018. The authors included adult patients with a diagnosis for prostate cancer, at least 1 claim for androgen deprivation therapy (ADT), diagnosis of metastasis before or within 90 days after ADT, and continuous eligibility for ≥6 months pre-index (defined baseline period) and ≥3 months post-index. The index date was defined as the date of first receipt of ADT or first receipt of novel hormonal therapy or docetaxel if initiated within 30 days before ADT. OS and HRU were assessed from the index date to the earliest of end of continuous eligibility, data availability, or death. The association between race and overall survival was evaluated with a multivariable Cox proportional hazards model and between race and HRU was evaluated with a multivariable Poisson model, controlling for age, plan type, region, median state income, residence in a state with Medicaid expansion, index year, Charlson comorbidity index (CCI), baseline HRU, and clinical characteristics.

The authors included 1,488 patients with mCSPC of whom 467 [31%] were Black or African American, 446 [30%] were White, 219 [15%] were Hispanic, and 356 [24%] were other races. Hispanic men were the oldest (mean age 68 years), followed by those of other races (67 years), White men (64 years), and finally Black or African American men (63 years).
Black or African American and Hispanic men had the highest CCI (0.6), followed by those of other races (0.5), and White men (0.4).
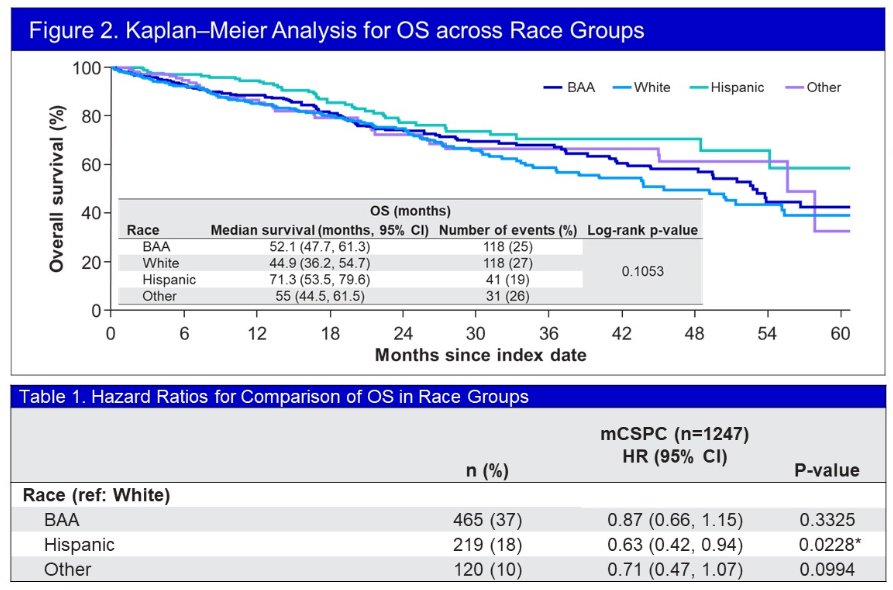
Median unadjusted OS was 71.3 months among Hispanic men, 57.1 months in men of other races, 52.1 months in Black or African American men, and 44.9 months in White men. After adjustment, Hispanic men had significantly lower risk of death compared to White men (hazard ratio [95% confidence interval (CI)]: 0.65 [0.43, 0.96]) and Black or African American patients had comparable survival to White men (0.91 [0.69, 1.22]).
Adjusted incidence rate ratios (IRR) showed significantly lower incidence of PC-related outpatient (OP) visits for Black or African American men as compared to White men (IRR [95% CI]: 0.71 [0.55, 0.99]), per patient per year. The remaining HRU endpoints were not significantly different among racial groups.

Thus, the authors concluded that, among Medicaid-insured adult patients with mCSPC, Hispanic men were more likely to live longer than White patients. Black or African American patients had similar survival and lower rates of PC-related OP visits as compared with White men, which shows differential use of PC-related healthcare resources between Black or African American and White men with mCSPC.
Presented by: Stephen J. Freedland, MD, Cedars-Sinai Medical Center

