(Urotoday.com) Germling genetic testing in prostate cancer has become more common as the relevance for patients grows, both in treatment planning and counseling of risk to family members. This has matched the expanded indications for germline testing in prostate cancer. Effective delivery of testing, including pre-test counseling, data interpretation, and patient education, is required. Interpretation of the patient experience through patient-reported outcomes (PROs) has been insufficiently studied.
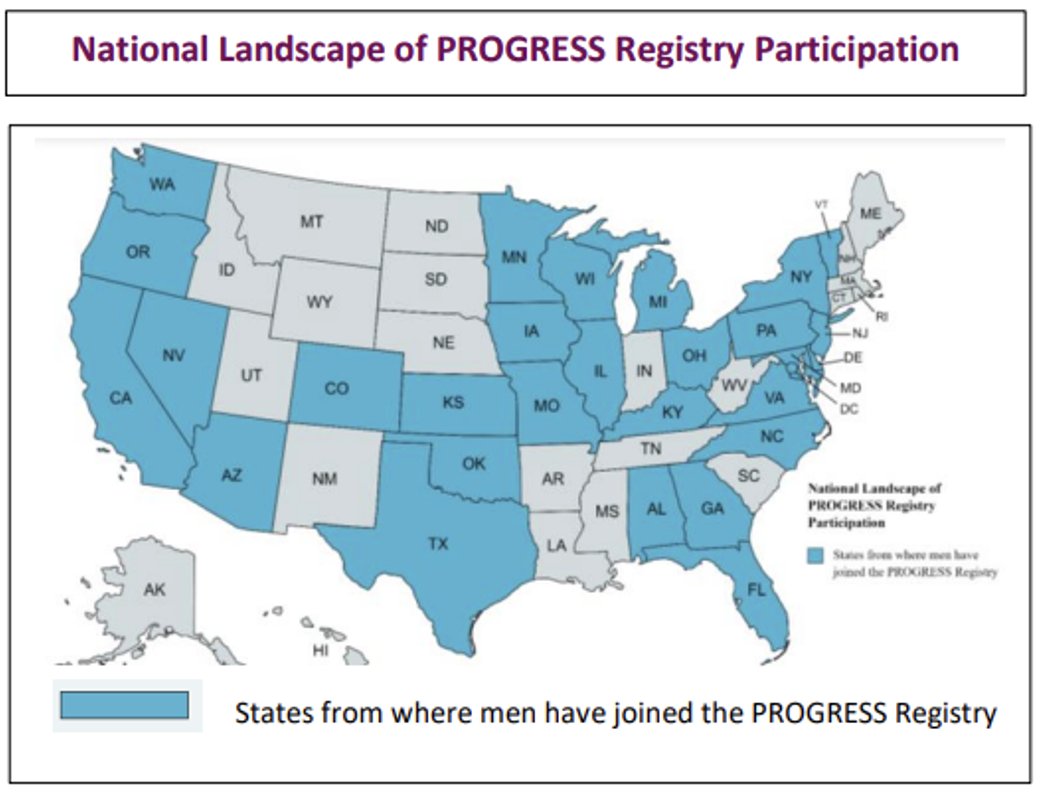
Dr. Veda Giri and colleagues, as presented by Dr. Whang Young, report on results of their PROGRESS Registry. PROGRESS (Prostate Cancer Genetic Risk, Experience, and Support Study) was developed to gain perspective on patient experience with germline testing in prostate cancer. The accrual goal of this ambitious multicentered registry was met (n=500), including patients from more than 25 states. Data collected, in addition to patient demographics, included prostate cancer history, mode of genetic evaluation, and measures of PROs (i.e., satisfaction, decisional conflict, attitude, knowledge of cancer genetics, medical literacy, and numeracy). Data were collected via online surveys and subjects received $50 compensation for completing them. Data were summarized using descriptive statistics. Multiple linear regression modeling assessed relationships between characteristics, mode of genetic evaluation, and PROs.
Among 414 with demographic data, a majority were White (87.7%) followed by Asian (6.0%). Most (87.7%) held a Bachelor’s degree or higher level of education. Most patients reported a first- or second-degree family member with any cancer diagnosis (74.6%), with 25.4% with that diagnosis being of prostate cancer. Approximately half of subjects reported a known diagnosis of prostate cancer. Among those subjects who reported their genetic results (n=416), 27.9% harbored a Pathogenic or Likely Pathogenic variant, 14.7% a Variant of Uncertain Significance (VUS), and 9.9% did not know.
Modes of genetic education included via a genetics profession (in-person, via phone, or via telehealth), by a doctor, from a website, from a video, and by a genetics lab. With regard to pre-test genetic education, 23.7% of patients reported not receiving any information prior to undergoing testing. The authors performed multiple regression models between testing-related data and PROs. Among the results highlighted include that satisfaction was lower in Asian as compared to White participants. Satisfaction was higher in those patients who received pretest information from a genetics professional via phone or from their doctor, as compared to other modes of delivery of pretest information. Decisional conflict, defined as personal uncertainty when deciding among choices with competing options involving risk, regret, or challenge to personal life values, was also variable.1 Decisional conflict was higher among Asian versus White participants, and higher for those participants who reported not knowing their genetic results, and lower for those who had genetic discussions with a genetics professional via phone.
The authors also reported that knowledge of cancer genetics was higher in those participants with higher education, family history of prostate cancer, those who received discussions from a genetics lab or from their doctors, and those with a Pathogenic/Likely Pathogenic alterations detected on germline testing.
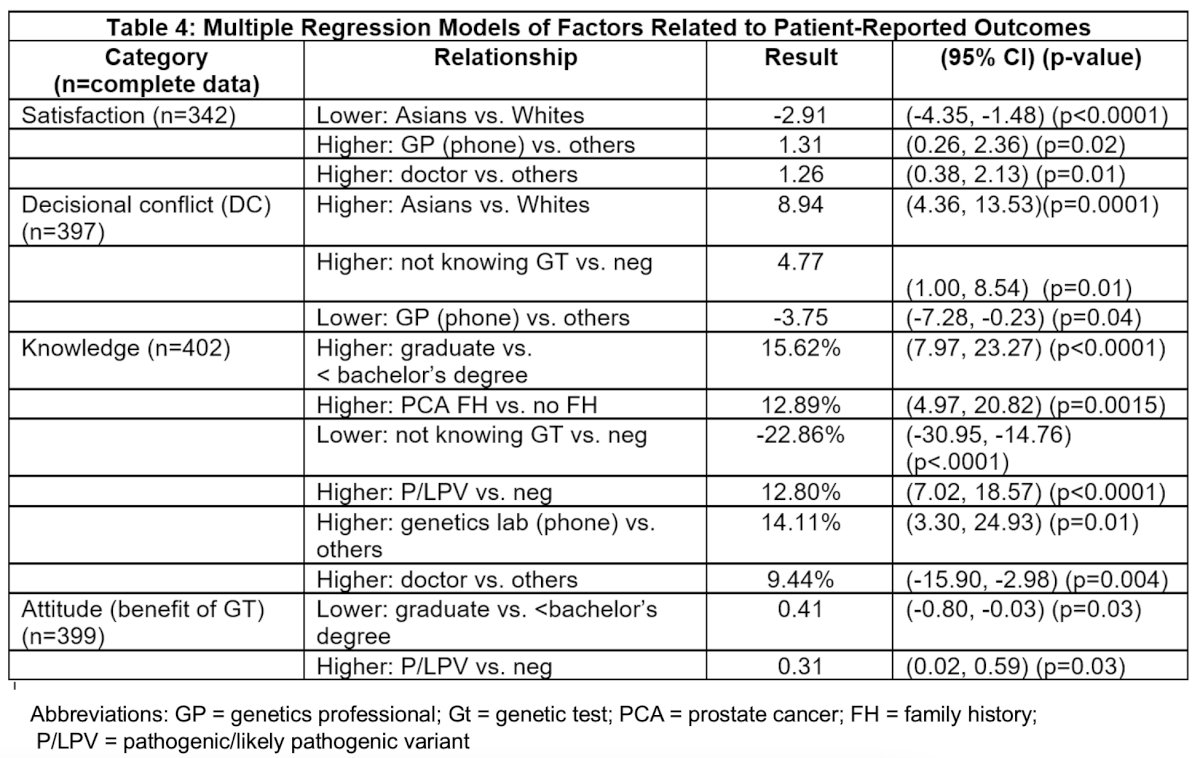
The PROGRESS conclude that the variety of factors that impact patient experience with germline testing in prostate cancer should warrant further evaluation of the root causes. In addition, they highlight that the high satisfaction and low decisional conflict among patients receiving genetic information via phone from a genetics professional supports the use of genetic counseling beyond in-person visits, as well as citing support for the point-of-care approach from a patient’s doctor. The authors also cite that differences between self-reported Race groups highlights the need to expand data collection and root cause analyses across diverse populations to assure genetics care delivery supports all men and their families.
Presented by: Young E. Whang, MD, PhD, University of North Carolina, Chapel Hill, NCWritten by: Jones Nauseef, MD, PhD, Assistant Professor of Medicine within the Division of Hematology and Medical Oncology, Sandra and Edward Meyer Cancer Center, and Englander Institute for Precision Medicine Weill Cornell Medicine and Assistant Attending physician at NewYork-Presbyterian Hospital. @DrJonesNauseef on Twitter during the 2023 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, Thursday Feb 16 – Saturday Feb 18, 20223
Reference:
- LeBlanc A, Kenny DA, O'Connor AM, Légaré F. Decisional conflict in patients and their physicians: a dyadic approach to shared decision making. Med Decis Making. 2009 Jan-Feb;29(1):61-8. doi: 10.1177/0272989X08327067. Epub 2009 Feb 4. PMID: 19196706.


