(UroToday.com) The 2023 American Society of Clinical Oncology Genitourinary (ASCO GU) cancers symposium held in San Francisco, CA between February 16th and 18th was host to a prostate cancer poster session. Dr. Sean Collins presented the results of his group’s study identifying prostate cancer patient subgroups based on their preferences for key attributes of androgen deprivation therapy (ADT).
Historically, ADT has been the standard of care for advanced PCa by causing a reduction in the levels of testosterone, with the foal of slowing PCa growth. Commonly used ADTs included injectable or implantable LHRH agonists and injectable GnRH antagonists. ADT usage/options have evolved to include several options varying in administration, adverse event profiles, T surge occurrence, speed of testosterone recovery, and costs. Data regarding patients’ preferences for ADT attributes remain limited.
This study included US men ages >40 years with healthcare coverage for the prior 3 years and self-reported PCa diagnosis, who were recruited via healthcare research panels to complete an online cross-sectional survey. Men were ineligible if they did not know or recall whether they had received ADT, were enrolled in a clinical trial, or were unable to complete the survey independently. Quotas ensured an approximately even split of ADT-experienced and ADT-naïve men. Preferences for ADT attributes were elicited using a discrete choice experiment involving a series of 11 choice tasks in which men were presented with 2 hypothetical ADT treatment profiles side-by-side and asked to select the one they preferred based on the following:
- Mode, frequency, and location of administration
- Testosterone surge
- Impact on sexual activity
- Cardiovascular event risk
- Normal testosterone after 3 months
- Out-of-pocket costs

Hierarchical Bayes models were used to compute attribute-level preference weights. Attribute relative importance (RI) was computed based on the difference between preference weights of the most and least favorable levels of each attribute, and then standardized to the sum of 100% across attributes. The higher the RI value, the more influential an attribute was to treatment choice. Preference heterogeneity was examined using latent-class analysis to identify potential subgroups within the sample that differed in their distribution of ADT attribute preferences:
- Multinomial logistic regression was conducted, with identification of the optimal latent class solution based on Bayesian Information Criteria
- Each individual was assigned to a class based on assignment probabilities
- Respondent characteristics were compared across the class assignments using 1-way ANOVA (continuous data) or chi-square tests (categorical data); p values<0.05, 2-tailed, were considered statistically significant
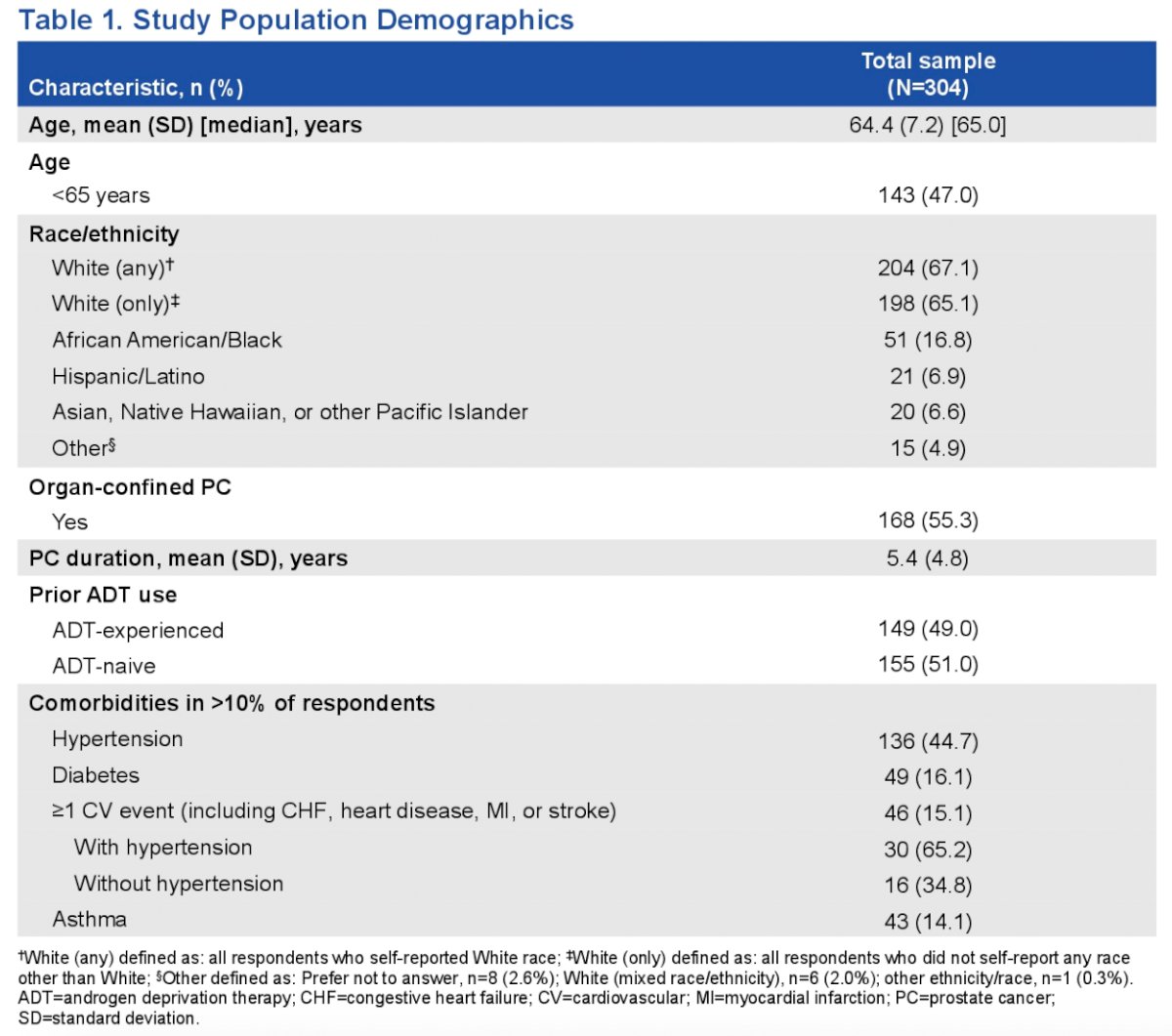
This study included 304 men with PCa. Mean age was 64 years, 65% were White, mean time from diagnosis was 5.4 years, 55% reported organ-confined disease, and 49% had prior ADT use. The most commonly reported comorbidity was hypertension.
Latent class analysis identified 4 subgroups differing in their attribute preferences:
- Group 1: Favors less impact on sexual activity and faster testosterone rebound
- Group 2: Favors infrequent ADT injection, slower testosterone rebound, and lower out-of-pocket costs
- Group 3: Favors once-daily ADT pill
- Group 4: Favors lower out-of-pocket cost

Attribute relative importance varied among the 4 preference subgroups:
- Group 1: Improvement in impact on sexual activity from ‘very much’ to ‘a little’ was most important (RI=32.0) and was 1.6 to 6.2 times more important than each of the other attributes
- Group 2: Reducing out-of-pocket costs from $350 to $5 (RI=24.1), changing from a once-monthly injection to a once-daily pill (RI=23.0), and increasing chance of testosterone recovery after discontinuation from 3% to 54% (RI=22.8), were perceived as being similarly high in importance
- Group 3: Changing from a once-monthly injection to a once-daily pill was most important (RI=40.1) and was 1.7 to 10.8 times more important than each of the other attributes
- Group 4: Reducing out-of-pocket costs from $350 to $5 was most important (RI=54.5) and was 3.6 to 14.0 times more important than each of the other attributes

The authors next evaluated for any difference in study population demographics by ‘latent class analysis’ groups 1 to 4:
- >50% of men in Groups 1 and 3 were <65 years old; Group 1, but not Group 3, mainly included men who planned to be sexually active
- Groups 2 and 4 were predominantly composed of men aged 65+ years (57.6% and 63.0%, respectively), who often had Medicare insurance (50.8% and 62.0%, respectively).
- The LCA subgroups were not significantly different according to ADT experience (p=0.622).

Dr. Collins concluded:
- When choosing PCa therapy, younger, sexually active men considered the potential impact on sexual activity
- Administration burden was the predominant driver of PCa treatment choice among younger men who were not often planning to be sexually active
- Some older men identified several PCa treatment attributes, including mode of administration and time to testosterone recovery, as important
- The subset of older men with Medicare insurance were highly sensitive to out-of-pocket costs when selecting PCa treatment
- Substantial variations in the salience of ADT attributes were observed among men with PCa, highlighting the need to take individuals’ preferences into account in shared decision-making
Presented by: Sean P. Collins, MD, PhD, Radiation Oncologist, Georgetown University Hospital, Washington, DC
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 Genitourinary (GU) American Society of Clinical Oncology (ASCO) Annual Meeting, San Francisco, Thurs, Feb 16 – Sat, Feb 18, 2023.


