(UroToday.com) On the second day of the American Society for Clinical Oncology (ASCO) Genitourinary Cancer Symposium 2023 focussing on urothelial cancer, the Poster Session B: Prostate Cancer and Urothelial Carcinoma included a presentation from Dr. Sean Fletcher examining oncologic outcomes for patients with residual invasive upper tract urothelial carcinoma (UTUC) following neoadjuvant chemotherapy.
It is often difficult to study patients with UTUC given its scarcity. For patients with advanced disease following radical nephroureterectomy, the POUT trial supports the use of adjuvant chemotherapy. However, many patients will be ineligible for cisplatin in this disease space. Thus, there is a growing body of literature supporting the use of neoadjuvant chemotherapy (NAC) prior to radical nephroureterectomy (RNU) for appropriately selected patients with upper tract urothelial carcinoma (UTUC). However, oncologic outcomes have not been well characterized for patients with residual muscle-invasive disease after NAC.
To address the issue, the authors leveraged a multi-institutional cohort from 24 centers in the U.S., Europe, and Japan to retrospectively identify patients who underwent RNU for UTUC from 1985-2022 and had high-grade muscle-invasive disease. They specifically compared patients who had residual muscle-invasive disease following NAC (>ypT2) as compared to those who did not receive NAC (>pT2). The authors excluded patients who received adjuvant chemotherapy, those who underwent concurrent cystectomy with RNU, and those with evidence of distant metastatic disease. They subsequently compared baseline characteristics between groups and then compared recurrence-free survival (RFS), overall survival (OS), and cancer-specific survival (CSS) using Kaplan-Meier survival analysis with log-rank test. Further, the authors used multivariable Cox regression and Fine-Gray competing risk regression were used to determine predictors of these outcomes.
The authors identified 1,233 patients, 62 of whom received NAC prior to RNU. A platinum-based regimen was used in 90% of NAC recipients, and the median number of cycles administered was 4 (IQR: 3-5). NAC recipients were more likely to have pathologic node positivity (35% vs. 13%) and less likely to have positive tumor margins (8% vs. 28%).
Over a median follow-up of 22 months (IQR: 8-47 months, Kaplan-Meier analysis demonstrated that NAC recipients with residual >ypT2 disease had poorer outcomes than those with >pT2 disease (2-year RFS [NAC vs. no NAC]: 52% vs. 80%, p<0.001; 2-year OS: 60% vs. 78%, p=0.003; 2-year CSS: 61% vs. 86%, p<0.001).

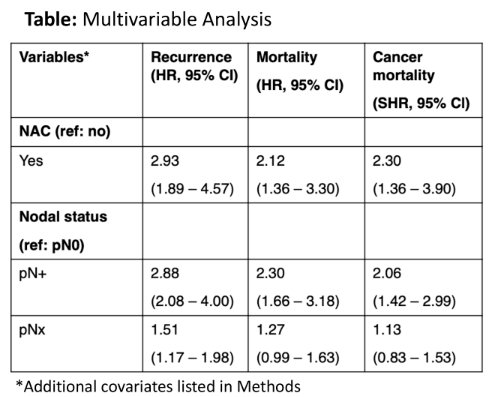
Multivariable analyses also showed a statistically significant association between residual muscle-invasive disease after NAC and poorer RFS, OS, and CSS.
Thus, the authors conclude that patients with UTUC who have residual muscle invasive disease following NAC have poorer outcomes than stage-matched chemotherapy naïve counterparts. This may reflect effects of occult micrometastatic disease or chemoresistant primary tumors in non-responders.
Presented by: Sean A. Fletcher, MD, Johns Hopkins Brady Urological Institute, Baltimore, Maryland

