(UroToday.com) The 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) cancers symposium held in San Francisco, CA between January 25th and 27th was host to a session on optimizing treatment strategies for patients with positive pelvic and/or retroperitoneal lymph nodes.
Dr. George Grass discussed the biology of tumor types among urologic oncology patients with positive pelvic/retroperitoneal lymph nodes and its implications for treatment selection with radiation versus surgery.
Dr. Grass began with a case presentation of a 52-year-old sexually active female who was diagnosed with multi-focal cT3bN2M1a disease with pure urothelial histology. She underwent 5 cycles of ddMVAC and had a complete response in all lymph nodes, partial response in the bladder (residual multi-focal), and a 220-fold decrease in ctDNA.
What are the clinical challenges remaining in this setting?
- How to manage residual bladder tumor after chemotherapy?
- How should pelvic nodal disease be best managed?
- Is there a role for consolidative radiotherapy in oligometastatic disease?
- How to best balance quality of life and treatment?
The goal of his talk was to present data from each anatomic site in order to guide treatment recommendations.
There is a clear lack of modern-day prospective studies with neoadjuvant chemotherapy (NAC) prior to bladder radiotherapy. Older studies published are limited by ‘outdated’ radiotherapy techniques with limited generalizability to modern day practice.
Numerous heterogeneous and retrospective studies have evaluated NAC followed by radiotherapy +/- chemotherapy. A recent systematic review demonstrated no difference in complete response rates (~75%) or 5-year OS between NAC followed by chemoradiotherapy versus chemoradiotherapy.1 As such, there is a clear need for more prospective data with modern radiotherapy and systemic therapy.
A recent phase 2 study from India evaluated the benefit of NAC prior to potential radiotherapy. This study included 40 patients (cT2: 45%, cT3N0: 40%; all male and urothelial histology). Patient underwent NAC with gem/cis x3 cycles. If patients had a complete or partial response ≥50% (defined by downgrading to cT1-2) with chemotherapy, patients underwent radiotherapy (+/- chemotherapy); otherwise, patients underwent a cystectomy. The primary endpoint of NAC response rate was recorded in 87.5% of patients (CR: 22.5%, PR ≥50%: 65%). 35/40 patients underwent radiotherapy (33 radiotherapy alone) with 46 Gy to the pelvis and a tumor boost to 66 Gy. They demonstrated that patients with a CR had a 30% improvement in the 3-year local control rate, compared to patients who achieved a partial response.2
What about other real-world data evaluating this approach?
What about management of clinically positive pelvic nodal disease? A recent retrospective analysis of 4 centers from the UK between 2012 and 201 evaluated radical versus palliative treatment approaches in 287 patients with cN+M0 disease. Radical therapy was defined by radical cystectomy +/- chemotherapy or radiotherapy/chemoradiotherapy. Palliative therapy could have included palliative radiation or chemotherapy. This trial included high-risk patient as demonstrated by the disease characteristics below:
- Radiotherapy group: 68% cT3/4 & 93% cN1-2 (69% receiving NAC)
- Cystectomy group:47% pT3/4 & 45% pN1-2 (42% w/o N status) with 45% receiving NAC
Patients in the radical treatment group had superior overall survival (p<0.0001). When radiotherapy and radical cystectomy patients were compared for survival outcomes, there was no significant differences between the two groups.3 These data suggested that there may be no detriment to offering a bladder sparing option in this poor prognosis population.

The IMPART trial was a phase II feasibility trial of chemoradiotherapy in LN positive disease. This trial included 38 patients with 60% having cN1-3 disease. 82% received NAC and 46% received chemoradiotherapy (3 received cystectomy). The primary endpoint was the feasibility to deliver intensity modulated radiotherapy (IMRT) using pre-defined radiotherapy planning goals, which was met and achieved in 76% of patients. The 5-year pelvic recurrence-free survival was 26%, and the median overall survival was almost 2 years with 34% of patients alive at 5 years. The bladder preservation rate was 85%. Late grade 3 gastrointestinal toxicity was observed in 5%. The distant metastasis risk remained high with this approach.
Do we offer consolidative radiotherapy to chemotherapy responders? There is limited data to guide optimized local therapy management after first-line systemic therapy. Two analyses from the NCDB have demonstrated that patients who received cystectomy (bottom left) or radiotherapy (bottom right) following initial chemotherapy had superior survival outcomes, compared to chemotherapy alone, although such registry analyses are ‘fraught’ with numerous potential selection biases.
A French study has recently evaluated the role of consolidative radiotherapy for patients with metastatic disease confined to the pelvis and retroperitoneal lymph nodes following 1st line chemotherapy. Patients in the active treatment arm received chemoradiotherapy or radiotherapy with >30 Gy, whereas those in chemotherapy only arm received either low doses of radiotherapy (<30 Gy) or no radiotherapy. As demonstrated below, patients in the chemoradiotherapy group had superior overall and progression-free survivals, supporting the role of consolidative therapy in this setting.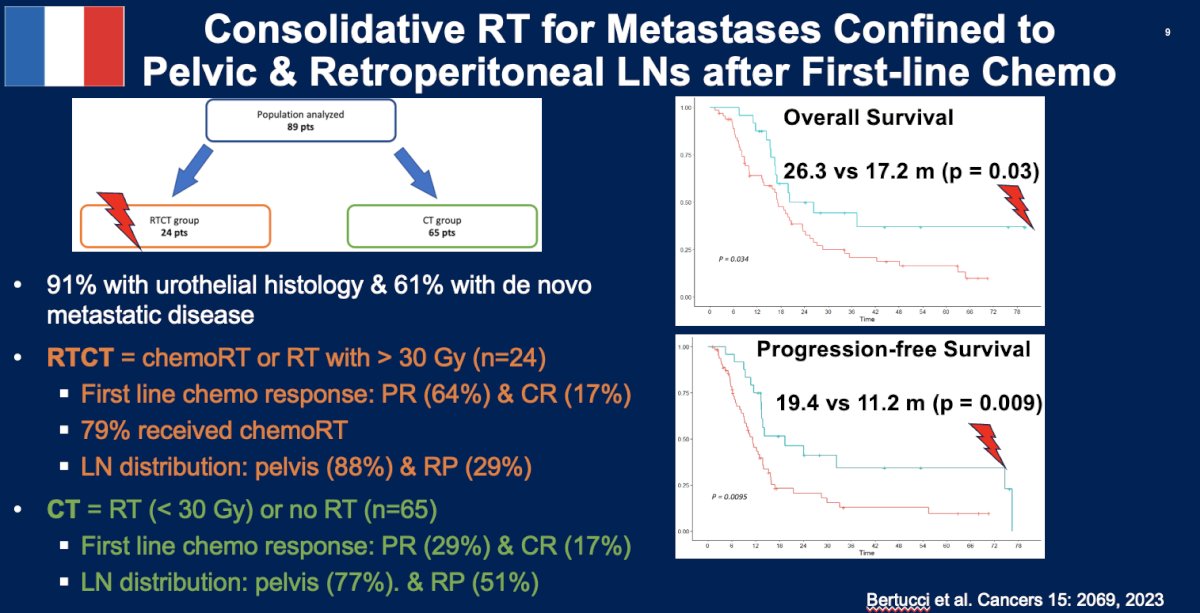
Currently, the BLAD-RAD01 trial is evaluating the role of consolidative radiotherapy for metastatic urothelial bladder cancer patients without progression and with ≤3 residual metastatic lesions following 1st line systemic therapy:
These clinical situations require a multi-disciplinary conversation. If not opting for radiotherapy for consolidation, patients could opt for either cystectomy or maintenance avelumab. If they elect for cystectomy, then their risk of local recurrence needs to be considered based on pathologic findings. If patients have intermediate- to high-risk of recurrence, then further therapy with radiotherapy could be considered. Alternatively, patients could opt for maintenance avelumab following 1st line platinum-based chemotherapy. However, the JAVELIN Bladder 100 trial demonstrated that despite survival improvements with avelumab, the median progression-free survival for such patients is still only 5.7 months.5 One thing to consider is whether these progressive events occur in the pelvis, where radiotherapy could be beneficial, or are distant in nature (systemic therapy preferable)?
While salvage radiotherapy may have local control benefits in this setting, there are numerous potential complications to carefully consider in this setting:
Dr. Grass noted that there also important considerations for radiotherapy and immunotherapy integration. Taken in isolation, radiotherapy is not ‘one size fits all’. The tumor response may be influenced by:
- Total RT dose
- Amount of RT dose delivered per fraction
- Spacing between RT doses
- Volume of target receiving RT dose
- Intrinsic tumor biology & RT interaction
In combination, radiotherapy may augment or diminish the immunotherapy effect:
- RT-mediated immunosuppression versus immunoactivation
- RT effect to draining lymph nodes
- Contribution of RT – sequencing or overlap
- Diverse RT parameters influence tumor-immune biology
The DUART (NCT02891161) is a phase II study (n=26) that evaluated the combination of durvalumab + radiotherapy in N+ patients. 30% of patients in this trial had N+ disease. Patients received durvalumab + radiotherapy for 7 weeks. At a median follow-up of 27 months, the 1-year PFS was 71.5%. Notably, there was no difference in PFS between N+ and N- patients, which may highlight the efficacy of such a combination in N+ patients. 6
What are some clinicopathologic and biologic factors to assist with bladder preservation selection? The “ideal” bladder preservation candidate is a patient meeting all of the following criteria:
- Urothelial histology
- cT2-T3a
- Unifocal
- Visibly complete TURBT
- < 5 – 7 cm
- No moderate/severe hydronephrosis
- No extensive CIS
- Good baseline bladder function
- cN0
- No prior pelvic RT
He concluded by noting that hypothesis-generating data suggests radical local therapy in cN+ or after response to first-line systemic therapy in oligometastatic patients may improve tumor control and survival outcomes. A patient-centered, multidisciplinary approach/collaboration is key to making such treatment decisions.
Presented by: George Daniel Grass, MD, PhD, Assistant Member and Clinical Investigator, Department of Radiation Oncology, Moffitt Cancer Center, Tampa, FL
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, San Francisco, CA, January 25th – January 27th, 2024
References:- Ding H, Fan N, Ning Z, Ma D, et al. Trimodal Therapy vs. Radical Cystectomy for Muscle-Invasive Bladder Cancer: A Meta-Analysis. Frontt Oncol. 2020;10:564779.
- Bracham CB, Kumar N, Kumar S, et al . A phase II study of neoadjuvant chemotherapy followed by organ preservation in patients with muscle-invasive bladder cancer. Asian J Urol. 2022;9(3):318-328.
- Swinton M, Mariam NBG, Tan JL, et al. Bladder-Sparing Treatment With Radical Dose Radiotherapy Is an Effective Alternative to Radical Cystectomy in Patients With Clinically Node-Positive Nonmetastatic Bladder Cancer. J Clin Oncol. 202341(27):4406-4415.
- Tan MP, Harris V, Warren-Oseni K, et al. The Intensity-Modulated Pelvic Node and Bladder Radiotherapy (IMPART) Trial: A Phase II Single-Centre Prospective Study. Clin Oncol. 2020;32:93-100.
- Powles T, Park SH, Voog E, et al. Avelumab Maintenance Therapy for Advanced or Metastatic Urothelial Carcinoma. N Engl J Med 2020 Sept 24;383(13):1218-1230.
- Joshi M, Tuanquin L, Zhu J, et al. Concurrent durvalumab and radiation therapy (DUART) followed by adjuvant durvalumab in patients with localized urothelial cancer of bladder: results from phase II study, BTCRC-GU15-023. J Immunother Cancer. 2023;11(2):e006551.


