(UroToday.com) The 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) cancers symposium held in San Francisco, CA between January 25th and 27th was host to a renal cell, adrenal, and testicular cancers rapid oral abstract session. Dr. Robert Huddart presented prognostic models for stage I seminoma within the randomized Trial of Imaging and Surveillance in Seminoma Testis (TRISST).
Dr. Huddart noted that, currently, stage I seminoma is typically managed with surveillance following a radical orchiectomy, with an estimated relapse rate of 15 to 20% with surveillance. However, salvage treatment for such patients who recur remains highly effective with survival outcomes approaching 100%. Adjuvant single-dose carboplatin can reduce the risk of relapse but remains unnecessary for the remaining 80 to 85% of patients who do not experience disease recurrence. As such, Dr. Huddart argued that there remains an unmet clinical need for effective risk stratification for patients with stage I seminoma. Historically, tumor size >4 cm and rete testis invasion have been identified as predictors of increased risk of disease recurrence;1 however, these may be out of date and have not been consistently validated. Recently, Boormans et al proposed a new EAU risk prognostication model based on tumor size (2, >2 – 5, and >5 cm), rete testis invasion, and lymphovascular invasion. Based on this classification, 56.4%, 41.3%, and 2.3% of patients would be classified as harboring low, intermediate, and high risks of disease relapse, with corresponding 5-year relapse rates of 8%, 20%, and 44%, respectively.2
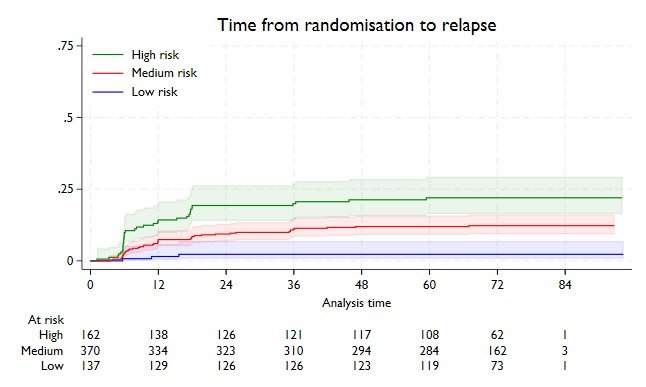
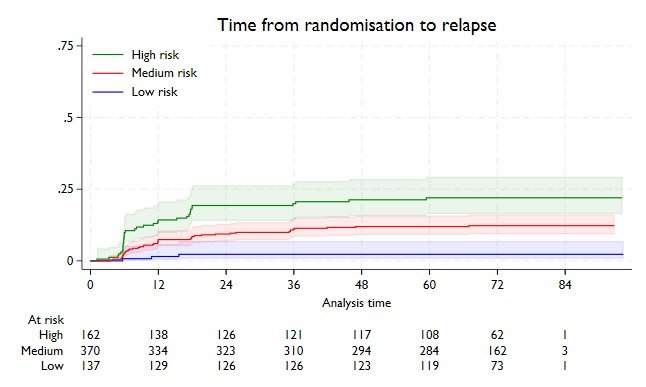
TRISST was a phase III factorial randomized controlled trial evaluating imaging schedules and modalities for the surveillance of stage I seminoma patients (n=669, 82 [12%] relapses). This trial demonstrated that a reduced surveillance schedule (three versus seven scans) and utilization of MRI (versus CT) are non-inferior to standard CT surveillance.3 Accordingly, Dr. Huddart and colleagues utilized individual patient data from the TRISST cohort to re-evaluate risk factors for disease relapse using multivariable Cox regression analysis and aimed to validate the EAU model by Boormans et al. within this cohort.
Utilizing the TRISST cohort data, Dr. Huddart and colleagues identified tumor size ≥4 cm (versus <2 cm: HR=4.0, 95% CI= 2.0-8.0) and pT3 disease (versus pT1: HR=3.9; 95% CI= 1.8- 8.6) as the clinical/pathologic variables most strongly associated with an increased rate of recurrence. Utilizing these two variables, along with patient age, they were able to define risk groups for predicting risk of disease recurrence as summarized below:
|
Risk group derived in TRISST |
% of cohort |
5-year relapse risk |
|
Low (age≥30 years, <2cm and pT1) |
20% |
2.3% |
|
Intermediate (age<30 years and/or 2-4cm and/or pT2@) |
55% |
12.0% |
|
High (≥4cm and/or pT3) |
24% |
22.0% |
With regards to validating the EAU model, Dr. Huddart and colleagues noted that the EAU model had a ‘good’ performance in the TRISST cohort, with a Harrell’s C-index of 0.62. Of note, the EAU ‘very high-risk’ group accounted for only 2% of the TRISST patient cohort, a major limitation.
|
EAU risk group applied to the TRISST cohort |
% of cohort |
5-year relapse risk |
|
Very low (≤5cm, no RTI, and no LVI) |
66% |
10.1% |
|
Low (≤2cm with RTI and LVI; OR 2-5cm with RTI and/or LVI; OR >5cm with not both RTI and LVI) |
33% |
16.1% |
|
High (>5cm with both RTI and LVI) |
2% |
45.5% |
Limitations to this analysis included the following:
- The patient population in the TRISST cohort was selected by local physicians who were recommending surveillance. Accordingly, patients perceived as ‘high risk’ may have been selectively managed by adjuvant chemotherapy, and the degree to which this happened may have varied from site to site.
- The proportions in each risk strata and factors predicting relapse may not represent the proportions in a whole patient population (i.e., more patients are actually high risk than recognized in the TRISST patient cohort).
- The TRISST prognostic risk stratification model ultimately requires independent validation in an external cohort.
Dr. Huddart concluded as follows:
- The relapse risk in stage I seminoma patients managed with surveillance is low for the vast majority of patients.
- Tumour size is consistently shown to be associated with an increased relapse risk.
- The EAU prognostic model identifies a small group (>5cm, with rete testis and lymphovascular invasion) with a particularly high risk who may benefit from adjuvant therapy.
- TRISST index identifies a larger high-risk group (~25%) with >20% relapse risk with all other patients harboring a <12% relapse risk.
Presented by: Robert A. Huddart, PhD, MBBS, FRCR, MRCP, Section of Radiotherapy and Imaging, Institute of Cancer Research and Royal Marsden NHS Foundation Trust, London, UK
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, San Francisco, CA, January 25th – January 27th, 2024
References:- Warde P, Specht L, Horwich A, et al. Prognostic factors for relapse in stage I seminoma managed by surveillance: a pooled analysis. J Clin Oncol. 2002;20(22):4448-52.
- Boormans JL, Sylvester R, Anson-Cartwright L, et al. Prognostic Factor Risk Groups for Clinical Stage I Seminoma: An Individual Patient Data Analysis by the European Association of Urology Testicular Cancer Guidelines Panel and Guidelines Office. Eur Urol Oncol. 2023; S2588-9311(23)00232-8.
- Joffe JK, Cafferty FH, Murphy L, et al. Imaging Modality and Frequency in Surveillance of Stage I Seminoma Testicular Cancer: Results from a Randomized, Phase III, Noninferiority Trial (TRISST). J Clin Oncol. 2022;40(22):2468-78.


