(UroToday.com) The 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) cancers symposium featured a prostate cancer session and a presentation by Dr. Peter Goebell discussing the underutilization of ADT intensification for the treatment of men with metastatic hormone-sensitive prostate cancer (mHSPC). Androgen deprivation monotherapy has been a cornerstone treatment for men with mHSPC since the mid-1940s. In the last decade (since early 2015), intensification of ADT with chemotherapy or androgen receptor pathway inhibitors has shown clinical benefits for men with mHSPC compared to ADT alone and has been recommended for mHSPC in clinical guidelines. Several studies have investigated the transition of these guidelines into real-world practice, however, these data have not been systematically summarized across the globe. As such, Dr. Goebell and colleagues conducted a systematic literature review of real-world database studies to summarize treatment patterns in mHSPC.
Eligible studies were retrospective or prospective observed real world database studies, including registries, claims electronic medical records, and chart reviews, examining ADT treatment patterns among men with mHSPC, covering the period from 2015 onwards. An electronic search was performed in PubMed and Embase (citations until July 2023) and for relevant conferences of the past two years to identify real-world database studies examining treatment patterns in men with mHSPC. First-pass screening retrieved citations conducted to determine eligibility according to defined criteria. Subsequently, a second pass screening was conducted by retrieving and reviewing the full-text articles to determine their final inclusion in the analysis. Treatment patterns were summarized by overall study population across major geographies and factors associated with ADT intensification were described.
Of 2,336 retrieved citations, 29 studies met the inclusion criteria, with 344,473 men with mHSPC covering study periods from 2014 to 2021. Most studies were cohort studies (n = 26), utilizing electronic medical records/chart reviews (n = 18), and with real-world databases from the United States (n = 21), followed by Europe (n = 8), and Asia (n = 6):
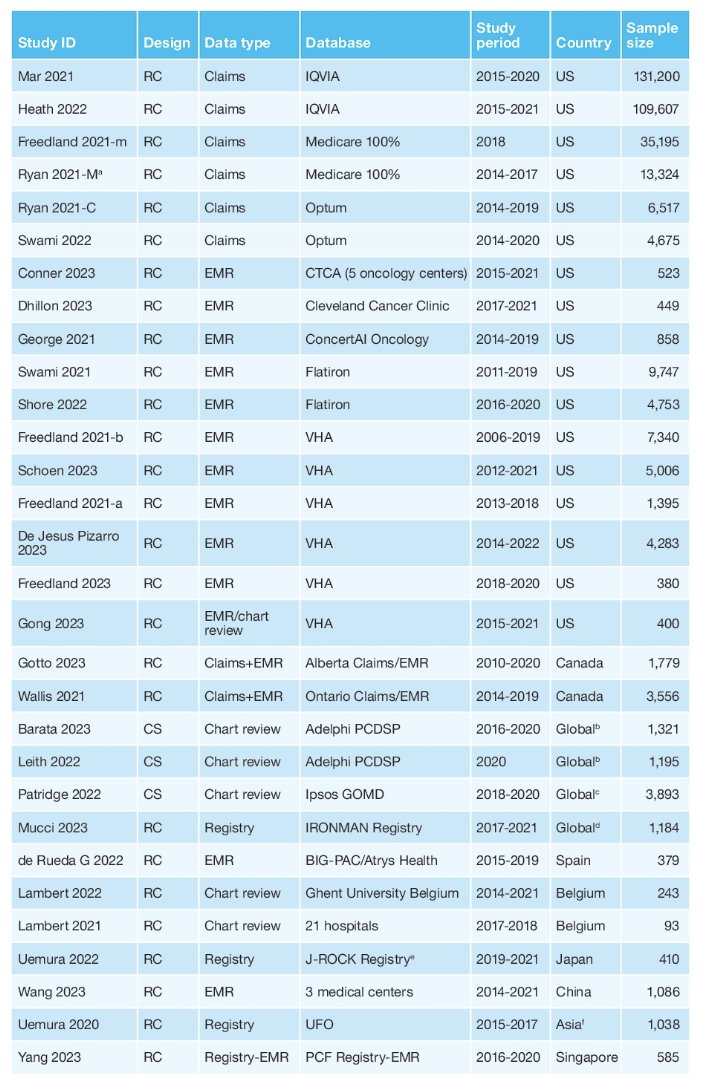
Most studies (n = 20) included men with a median age of ≥70 years and >80% of men had an Eastern Cooperative Oncology Group performance status of 0 or 1 (5 of 8 studies). In the United States and Canada, ADT monotherapy was predominantly utilized (most studies >50%), followed by ADT + androgen receptor pathway inhibitors (20-40%), and ADT + docetaxel (10-20%). Abiraterone was the most frequently used androgen receptor pathway inhibitors followed by enzalutamide. In Europe, most studies also reported ADT monotherapy (>40%), followed by ADT + androgen receptor pathway inhibitors (13-38%), or ADT + docetaxel (12-36%). In Asia, ADT monotherapy (>62%) was the most common treatment in most studies, with low use of ADT + androgen receptor pathway inhibitors (<20%), and ADT + docetaxel (<15%):

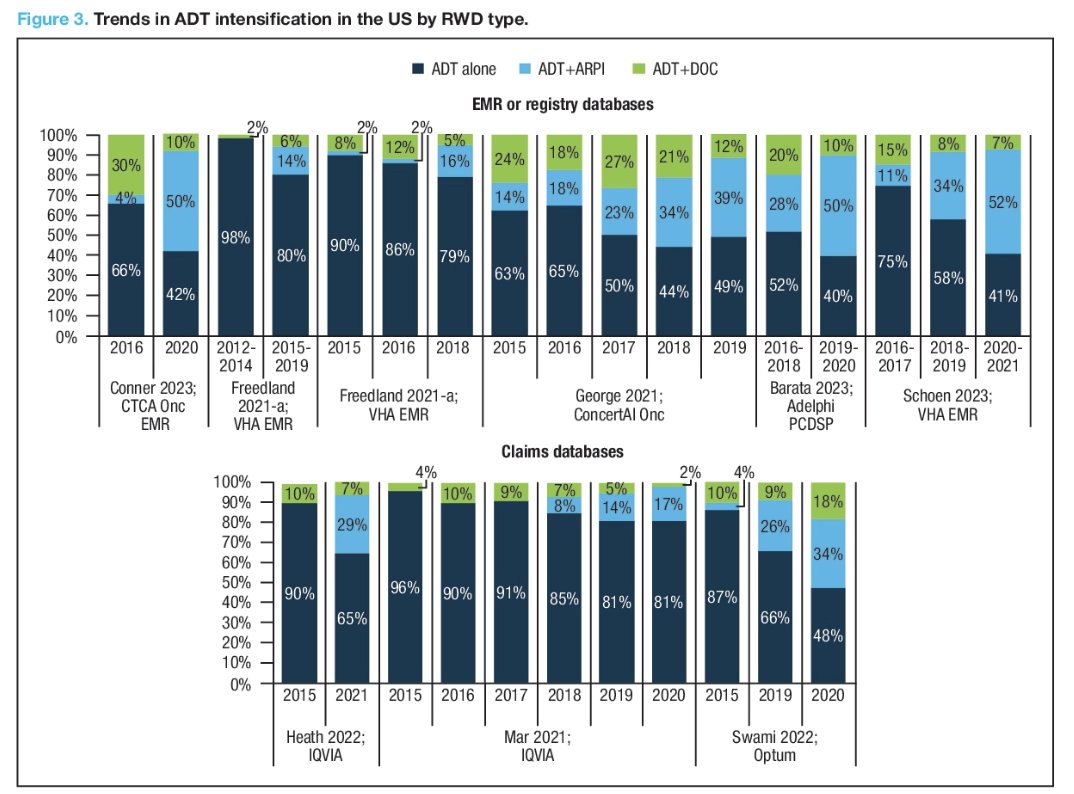
All studies showed an increasing trend in ADT/androgen receptor pathway inhibitor use from 2015 to 2021, although the magnitude of the increase varied by source. Overall ADT/docetaxel remained fairly consistent over time:
In the IRONMAN Registry, ADT + androgen receptor pathway inhibitors made up nearly 2/3 of treatment use across the US (58%) and Canada (67%), whereas the use of ADT monotherapy (US: 25%, Canada: 17%) and ADT + docetaxel (US: 17%, Canada: 16%) was substantially lower:
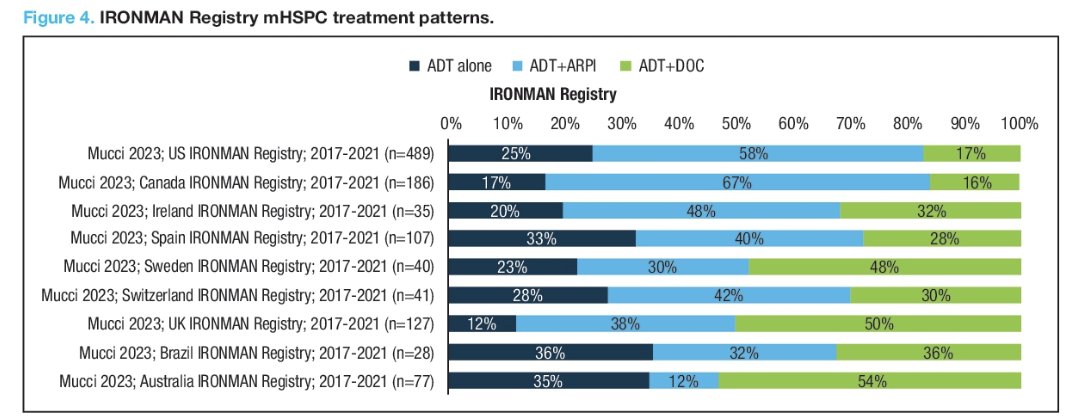
Less ADT + androgen receptor pathway inhibitor and ADT + docetaxel use were observed in men with mHSPC who were treated by urologists versus oncologists, and there are national differences in who is providing more complex systemic treatment (hospital vs office based; urologist vs oncologist). ADT + androgen receptor pathway inhibitor use was greater in men with high-volume and high-risk mHSPC than in their counter populations. Abiraterone remained the primary androgen receptor pathway inhibitor in combination with ADT (up to 40% of patient cohorts) in the US, Canada, Europe, and Asia in most studies. In contrast, enzalutamide use was low and limited to <= 20% of the mHSPC population in most global studies. Apalutamide use was reported in only a few studies and remained low (<7%) with a few exceptions.
Reported quantitative factors (n = 13) associated with intensification beyond ADT were:
- High disease burden (spread of metastases, high volume)
- Young age
- Eastern Cooperative Oncology Group performance status 0 or 1
- Low comorbidities
- Treating physician specialty-oncologist
Qualitative factors (n = 2) were patient preference, unsatisfactory response to ADT treatment, ability to tolerate adverse events, and lack of cost barriers.
Dr. Goebell concluded his presentation by discussing the underutilization of ADT intensification for the treatment of men with mHSPC with the following take-home points:
- This is the most up-to-date systematic review of the literature summarized treatment patterns of men with mHSPC using data from 29 real world studies across the globe, covering data up to 2021 and representing 344,473 men
- This review highlighted an increasing trend in ADT intensification (particularly with androgen receptor pathway inhibitor agents) over the study period across different geographies, however, the use of ADT intensification remains suboptimal considering the high proportion of patients still receiving ADT monotherapy, particularly in the US
- There remains an unmet need for further research to help understand how to optimize the adoption of guideline-concordant therapies alongside greater awareness and educational intervention of current therapies in mHSPC
Presented by: Peter J. Goebell, MD, PhD, University Clinic Erlangen, Erlangen, Germany
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, San Francisco, CA, January 25th – January 27th, 2024


