(UroToday.com) The 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) cancers symposium held in San Francisco, CA between January 25th and 27th was host to a prostate cancer poster session. Dr. Stacy Loeb presented the IMPLEMENT study evaluating barriers and facilitators to first-line treatment intensification in patients with metastatic castration-sensitive prostate cancer (mCSPC).
Despite the abundance of evidence for treatment intensification with androgen receptor pathway inhibitors and/or docetaxel in the 1st line treatment setting for mCSPC patients, and current guidelines unanimously recommending doublet/triplet therapy approaches for the 1st line management of such patients, there is a significant implementation gap with underutilization of such approaches in clinical practice.1,2 In the IMPLEMENT study, Dr. Loeb and colleagues evaluated barriers and facilitators to mHSPC treatment intensification that US urologists and oncologists face and identified behavior change techniques that may address these, using an implementation science approach.
Accordingly, the investigators performed 36 double-blind, semi-structured, virtual interviews with 36 practicing US urologists and oncologists, who manage mCSPC patients, using an interview guide, based on the theoretical domains framework. When no new themes emerged, saturation was considered met.
Barriers and facilitators were identified by coding physician statements into 11 domains. To confirm codebook reliability, 10% of transcripts were double coded independently (k=0.77). Key domains and the associated barriers and facilitators were analyzed for frequency, perceived potential to impact behavior, and presence of disagreement. Top domains were cross-referenced with a taxonomy of validated behavior change techniques.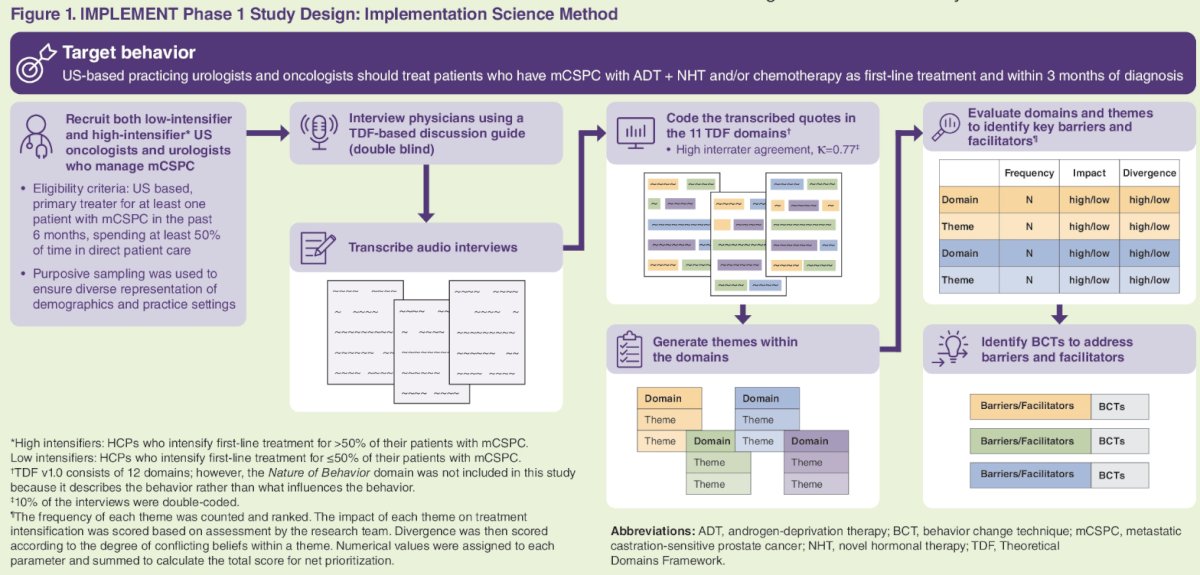
In total, 36 physicians were interviewed, of whom 20 were considered ‘low intensifiers’ (i.e., ≤50% of patients get treatment intensification), and 16 were classified as high intensifiers (i.e., >50% of patients get treatment intensification). 14/36 (39%) patients were from academic centers.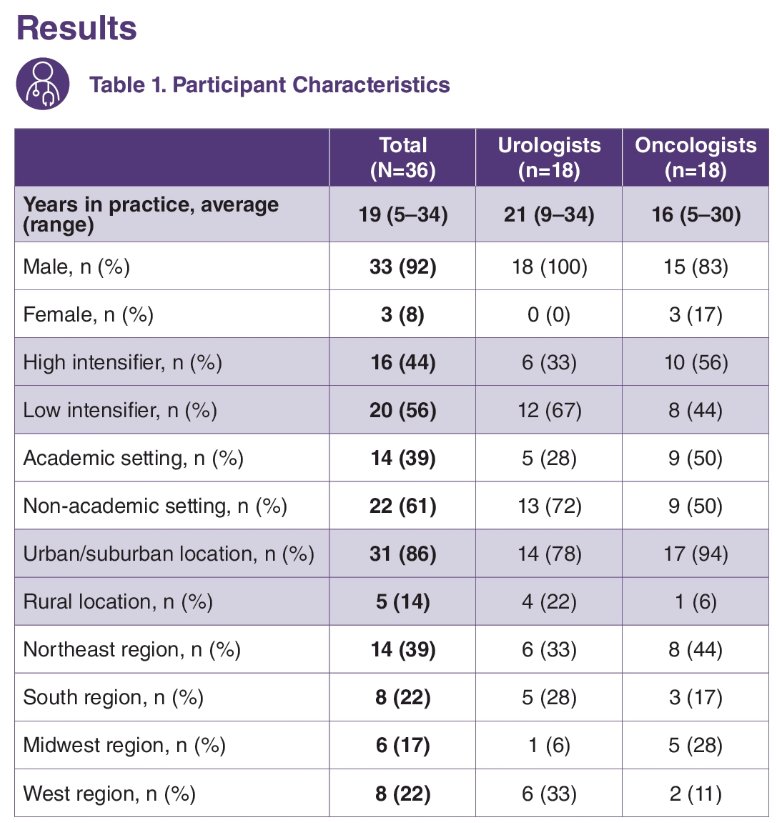
Dr. Loeb and colleagues were able to identify five impactful domains, along with the associated barriers, facilitators, and behavior change techniques relevant to each domain:
- Knowledge
- Belief about consequences
- Decision processes
- Social/professional role
- Environmental


Dr. Loeb concluded that underutilization of treatment intensification in US is multifactorial in etiology. The most prominent barriers included: poor knowledge, habit, anticipated regret, costs, and reserving treatment intensification for later use. She argued that these barriers can be addressed through behavior change techniques to improve early mCSPC treatment intensification.
Presented by: Stacy Loeb, MD, Professor of Urology and Population Health at NYU Langone Health and the Manhattan Veterans Affairs, New York, NY
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, San Francisco, CA, January 25th – January 27th, 2024
References:- Ryan CJ, Ke X, Lafeuille M, et al. Management of Patients with Metastatic Castration-Sensitive Prostate Cancer in the Real-World Setting in the United States/ J Urol. 2021;206(6):1420-1429.
- Freedland SJ, Sandin R, Sah J, et al. Treatment patterns and survival in metastatic castration-sensitive prostate cancer in the US Veterans Health Administration. Cancer Med. 2021;10(23):8570-8580.


