(UroToday.com) The 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) cancers symposium held in San Francisco, CA was host to a prostate cancer poster session. David Gelikman presented the results of a study evaluating the effect of urinary stagnation in the prostatic urethra on the generation of false-positive midline lesions with 18F-DCFPyL PSMA PET/CT scans.
Owing to its improved diagnostic performance compared to conventional imaging methods,1 PSMA-PET-CT has become increasingly utilized for patients with localized prostate cancer. However, this imaging modality is limited by radiotracer uptake in the ureters, bladder, and urethra secondary to physiologic urinary excretion. PSMA activity within the prostatic urethra can mimic midline intraprostatic lesions, if not carefully evaluated on MRI. This study aimed to evaluate the correlation between positive 18F-DCFPyL activity in the midline prostate with hyperintense signal on T2-weighted MRI, indicative of retained urine in the prostatic urethra.
The investigators retrospectively collected PSMA PET/CT and MRI images of patients with localized, clinically significant prostate cancer. PSMA activity in the midline region of the prostate was prospectively evaluated by one of two nuclear medicine physicians. Post-void T2-weighted MRI images were retrospectively evaluated for presence of residual urine noted by hyperintensity within the prostatic urethral lumen by one expert genitourinary radiologist. The prostatic urethra was measured in both the axial and sagittal planes on T2-weighted MRI. Patients without hyperintensity were measured as 0 mm. MRI and PET/CT findings were compared using Fisher’s exact and Mann-Whitney U tests.
This analysis included 84 patients. Midline PSMA activity was noted in 16 patients (case group), whereas no activity was found in the remaining 68 patients (control group). Of the 16 patients in the case group, 12 (75%) had prostatic urethral hyperintensity on T2-weighted MRI, whereas 31% of patients in the control group (i.e., no midline PSMA activity) had prostatic urethral hyperintensity on T2-weighted MRI (p<0.01). For patients with hyperintense urethral lumen on MRI, there was a significant difference in mean prostatic urethral measurements between case and control groups in the axial (7.25 mm versus 2.81 mm, p<0.0001) and sagittal planes (12.25 versus 5.43 mm, p<0.001).
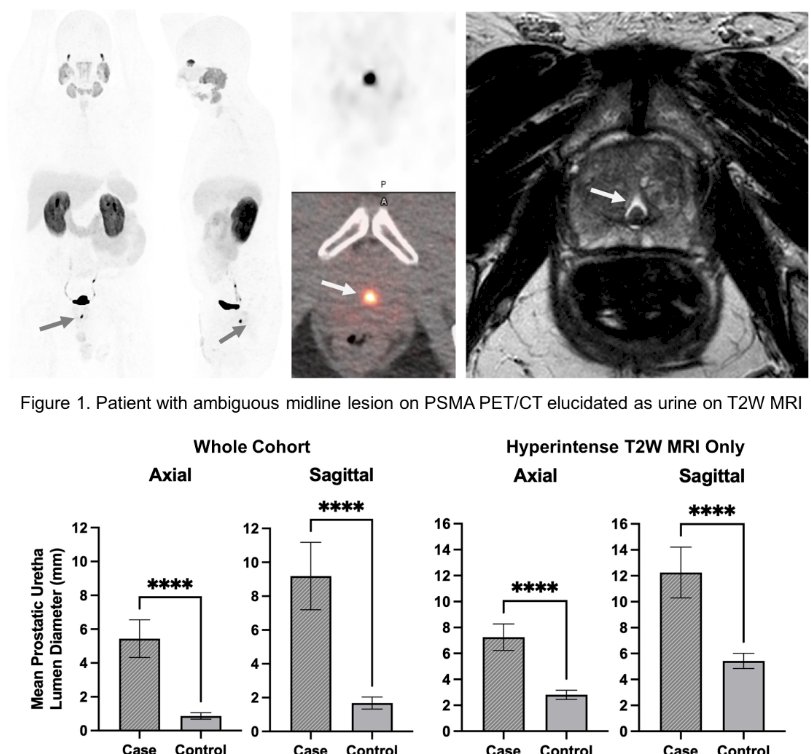
The presenter concluded that PSMA uptake in the prostatic midline is more commonly observed in patients with a prominently visible prostatic urethra on MRI, likely secondary to retained urine containing PSMA radiotracer. One potential solution is the use of post-void MRIs to reduce false positive interpretations of PSMA-PET/CT.
Presented by: David G. Gelikman, BA, Research Fellow, Molecular Imaging Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, San Francisco, CA, January 25th – January 27th, 2024
References:
- Hofman MS, Lawrentschuk N, Francis, RJ, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): A prospective, randomized, multicentre study. Lancet 2020 Apr 11;395(10231):1208-1216.


