The 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) cancers symposium held in San Francisco, CA between January 25th and 27th was host to a prostate cancer poster session. Dr. Egesta Lopci presented the interim analyses of the PROSPET-BX trial comparing 68Ga-11-PSMA PET/CT to multiparametric MRI (mpMRI) in patients with a previous negative prostate biopsy who remain at high suspicion for prostate cancer.
The PROSPET-BX trial aimed to prospectively compare 68Ga-PSMA-11 PET/CT with mpMRI in men with a high suspicion of prostate cancer (PCa) after at ≥1 previous negative biopsy. Between April 2022 and September 2023, 94 patients were screened, of whom 78 were enrolled and 64 completed all study investigations. The study inclusion criteria were as follows:
- PSA >4 ng/ml
- Free-to-total PSA ratio <20%
- Two consecutive PSA level measurement increases
- ≥1 prior negative biopsy
- Negative digital rectal examination
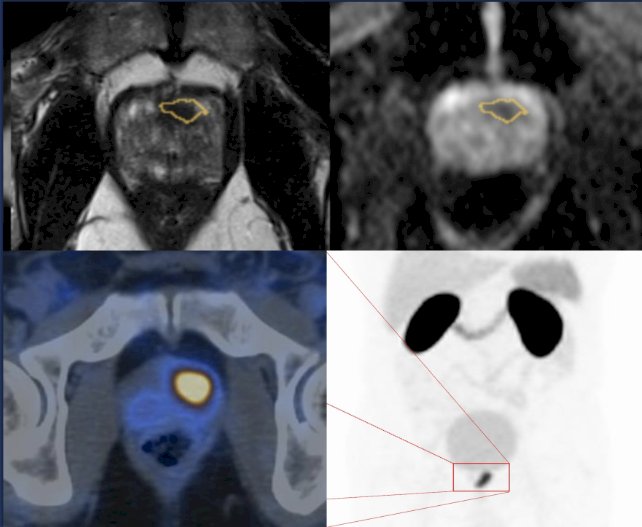
Both 68Ga-PSMA-11 PET/CT and 3T mpMRI were performed within one month of each other, followed by a TRUS-fusion prostate biopsy. Target lesions by imaging modality were defined by the following scoring systems:
- PI-RADS v2.1 for mpMRI
- PRIMARY Score, SUVmax, and SUVratio for PSMA-PET/CT
The median patient age was 64 years (range: 51 to 83), and the median PSA level was 10.4 ng/ml (range: 4.3 – 25.9 ng/ml). Consistent with the eligibility criteria, most patients (77%) had one prior negative biopsy. On repeat biopsy, 10/94 patients had clinically significant prostate cancer, 4/94 had evidence of Grade Group 1 disease, and the remainder (78%) had a negative biopsy.
Results of the mpMRI by PIRADS v2.1 score were as follows:
- PIRADS 2: 63%
- PIRADS 3: 5%
- PIRADS 4: 23%
- PIRADS 5: 9%
The PRIMARY scores were as follows:
- 1 to 2: 70%
- 3 to 5: 20%
In this trial, the PIRADS and PRIMARY scores were found to be significantly correlated (p<0.001). The median SUVmax and SUVratio were 3.7 and 1.35 for benign versus 8.9 and 3 for malignancy, respectively (p<0.001).
Receiver operating characteristic (ROC) curve analyses identified optimal cut-off points for clinically significant prostate cancer, with SUVmax>7.48 (AUC: 0.76; 95%CI: 0.63 - 0.86) and SUVratio >2.79 (AUC: 0.75; 95%CI: 0.62 – 0.85). PI-RADS, Primary score, SUVmax, and SUVratio were demonstrated to be significantly associated with biopsy results.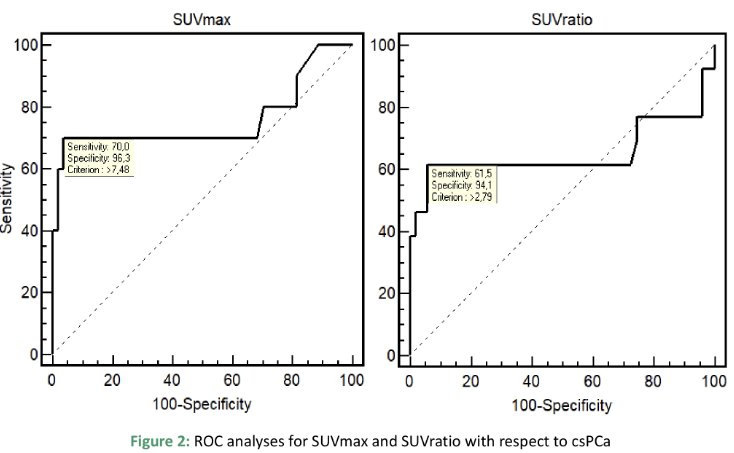
When mpMRI and PSMA-PET/CT data were combined, the detection rate (i.e., sensitivity) was 90% for clinically significant prostate cancer, and the combination of both modalities could spare 87.5% unnecessary re-biopsies.
Dr. Lopci concluded that these interim results suggest that 68Ga-11-PSMA PET/CT parameters predict biopsy results similarly to mpMRI in patients who are candidates for a repeat. He suggested that the combination of both modalities can spare most unnecessary repeat biopsies, given the high combined sensitivity/detection rate of 90%.
Presented by: Egesta Lopci, MD, PhD, Nuclear Medicine, IRCCS - Humanitas Research Hospital, Lombardia, Italy
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, San Francisco, CA, January 25th – January 27th, 2024


