(UroToday.com) The 2024 GU ASCO annual meeting featured a session examining the emerging evidence in localized and recurrent prostate cancer, including a presentation by Dr. Alan Dal Pra discussing salvage radiotherapy options for biochemical recurrence after local treatment.
Dr. Dal Pra started by highlighting that there are important aspects to consider when discussing salvage radiotherapy for biochemical recurrence after a prostatectomy versus salvage radiotherapy for biochemical recurrence after radiotherapy. After a prostatectomy, it is important to consider: (i) the timing of salvage radiotherapy after biochemical recurrence, (ii) use and duration of ADT with salvage radiotherapy, (iii) adding prophylactic pelvic nodal radiation, (iv) radiotherapy dose escalation, (v) shortening treatment (hypofractionation), and (vi) assessing genomic biomarkers. After radiotherapy, it is important to consider: (i) the importance of local recurrence, (ii) performing a workup for local recurrence, (iii) treatment options, (iv) outcomes with salvage brachytherapy + Stereotactic body radiation therapy (SBRT), and (v) several uncertainties and ongoing clinical trials.
Starting with salvage radiotherapy for biochemical recurrence after prostatectomy, Dr. Dal Pra notes that there have been changes in the primary management of localized prostate cancer over the years. For low-risk disease, there is an increasing use of active surveillance, no major changes for intermediate risk disease, but for high-risk patients, there is an increasing utilization of radical prostatectomy, which has led to a higher rate of biochemical failures requiring salvage treatment: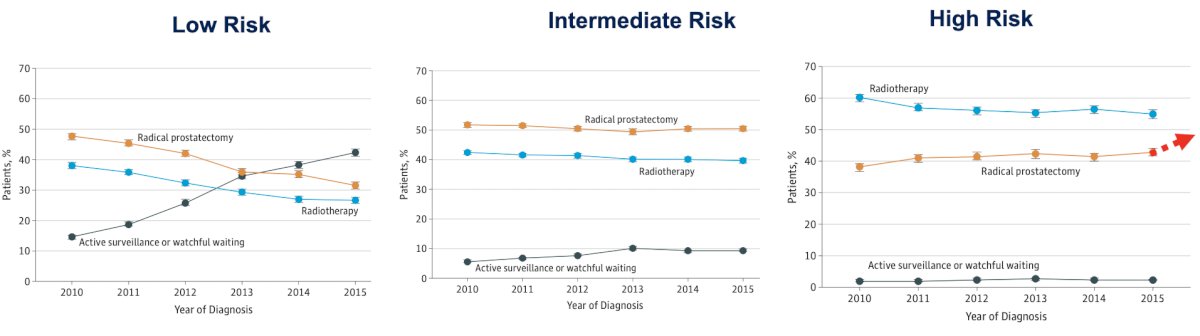
Salvage radiotherapy has been considered the only potentially curative therapy after biochemical failure and has been associated with better outcomes if given at lower PSA levels. In fact, Tilki and colleagues recently showed that salvage radiotherapy when given at a PSA equal to or lower than 0.25 ng/mL is associated with improved all cancer-mortality:1
In a phase 3 clinical trial from Japan, patients with BCR were randomized (median PSA 0.48 ng/mL) to salvage hormone therapy vs local treatment with salvage radiation therapy ± hormone therapy group.2 At a median follow-up of 5.5 years, patients treated with salvage radiotherapy had an increased time to failure compared to salvage hormonal therapy only: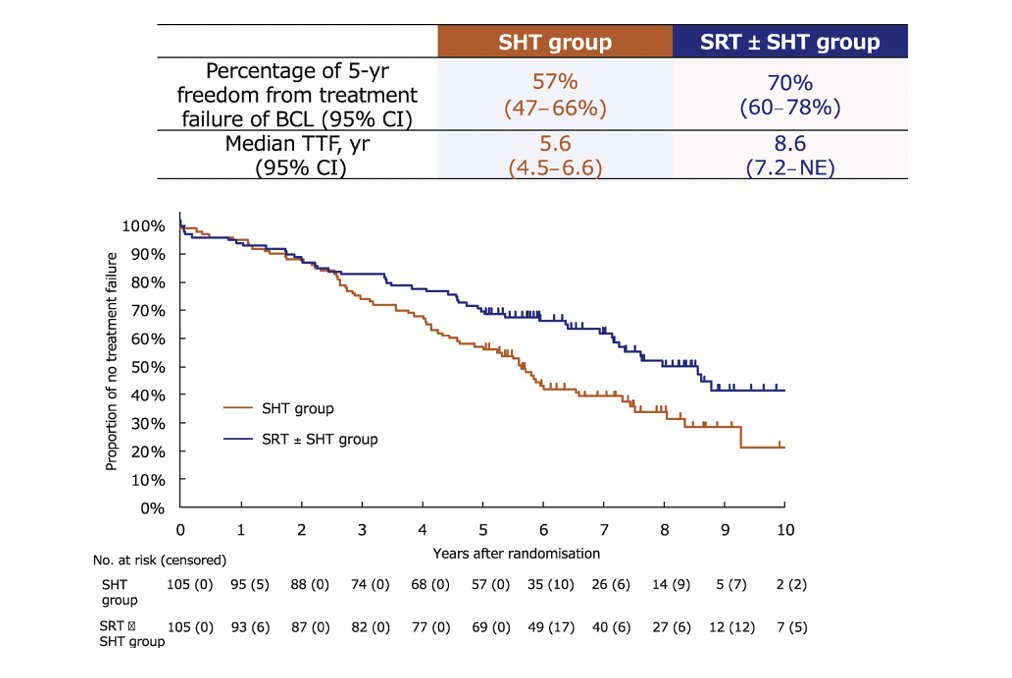
However, despite the data favoring salvage radiotherapy, Dr. Dal Pra notes that only 1 in every 6 patients with recurrent prostate cancer receive early salvage radiotherapy according to data from the MUSIC collaborative: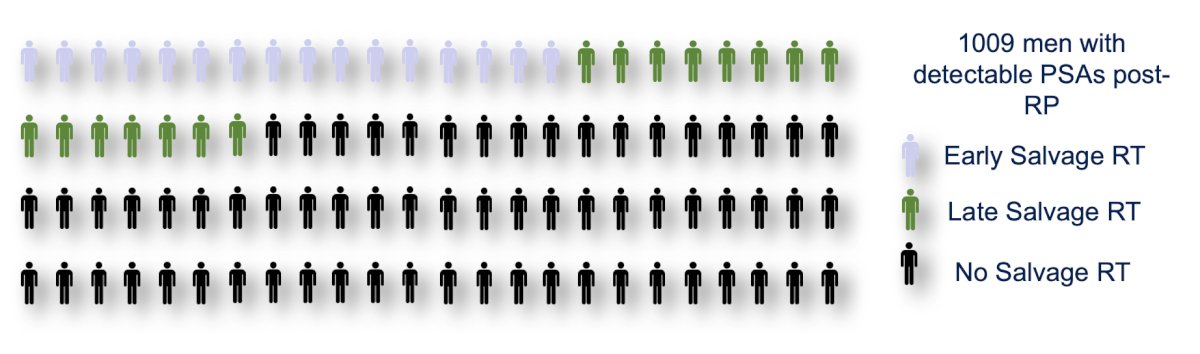
PSMA PET/CT imaging has importantly changed the landscape of biochemically recurrent patients, modifying management in more than 50% of the cases, and ongoing studies will confirm if these changes can lead to improved clinical outcomes. However, we need to keep in mind that PMSA PET/CT has limitations at low or very low PSA levels, and these are the same limitations as any other PET tracer. The following figure shows 10^7 cells with FDG uptake and PET was not able to detect a lesion, therefore we might be seeing only the visible part of the iceberg on PSMA PET/CT: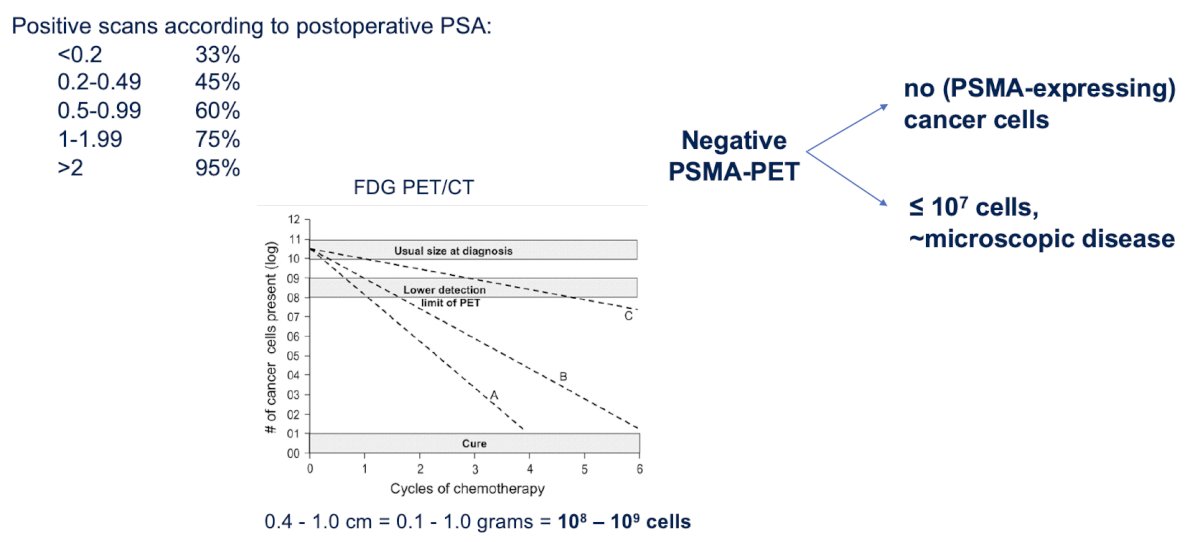
Dr. Dal Pra emphasized that there are studies showing that the outcomes of patients after salvage radiotherapy are much better in patients who have a negative PSMA PET/CT scan. Patients with a completely negative scan do better when they are treated with salvage radiotherapy to the prostate bed than when they are observed, which is reflected in a strong recommendation in the EAU guidelines that a negative PSMA PET/CT should not delay salvage radiotherapy if otherwise indicated: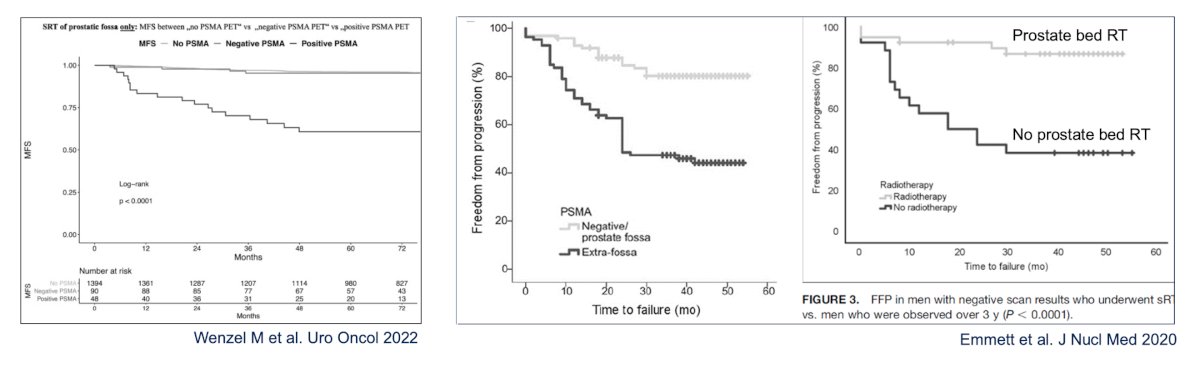
Dr. Dal Pra then discussed whether we should use ADT with salvage radiotherapy and if so, what should be the duration of ADT? Starting with RTOG 9601, this trial randomized patients with biochemical failure to 24 months of bicalutamide or placebo, including patients with a median PSA of 0.6 ng/mL, as well as allowing patients with a persistent PSA after radical prostatectomy.3 At a median follow-up of 13 years, there was a 4% benefit in overall survival: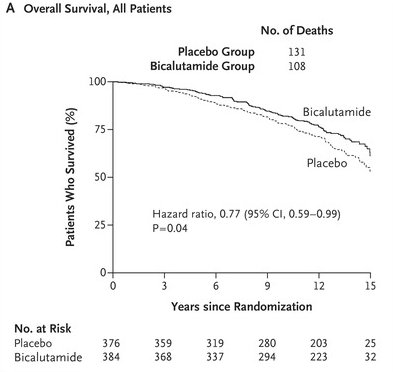
A subsequent analysis of RTOG-9601 showed that not all patients benefited equally from hormone therapy, and in fact, some may be harmed: in patients receiving early salvage radiotherapy (PSA ≤ 0.6 ng/mL), there was no improvement in overall survival and an increased likelihood of late grade 3 or higher cardiac and neurologic toxic effects with an increased risk of other-cause mortality. The GETUG 16 study, randomized patients with a median PSA after prostatectomy of 0.3 ng/mL to salvage radiotherapy to the prostate bed with or without 6 months of ADT.4 At a median follow up of 9.3 years, the progression free survival was superior in patients receiving ADT (HR 0.54, 95% CI 0.43-0.68). Additionally, there was a statistically significant benefit in metastasis free survival at 10 years and there was no benefit in overall survival: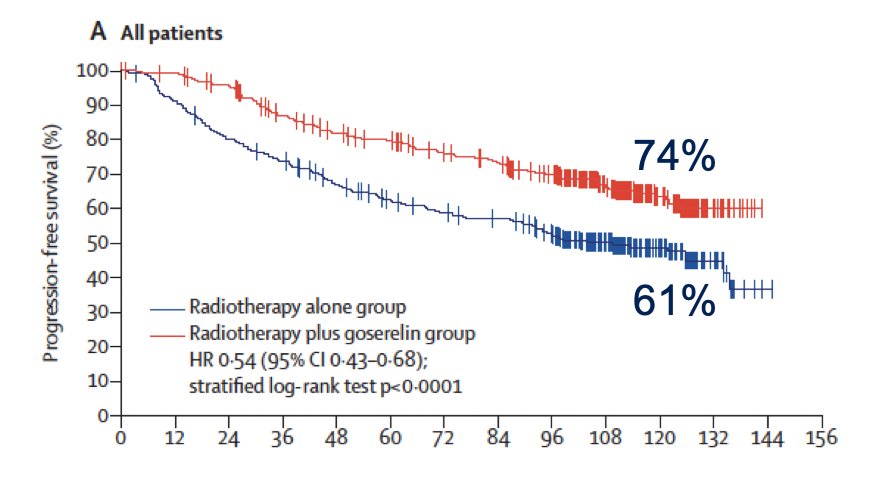
Next, the SPPORT trial randomized 1,716 patients with biochemical recurrence after surgery to prostate bed alone vs prostate bed + 6 months of ADT vs prostate bed, 6 months of ADT, and elective treatment of the pelvic lymph nodes. At a median follow up of 8.2 years, there was an incremental benefit in freedom from progression with treatment intensification from 71% arm to 81% in arm 2 and 87% in arm 3: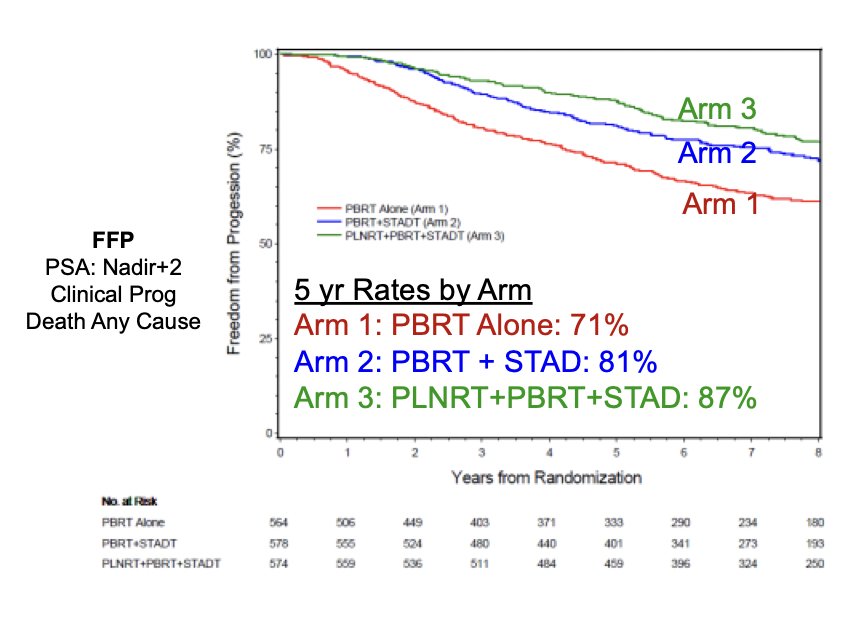
Additionally, there was a statistically significant benefit in second salvage ADT and no benefit in metastasis free survival or overall survival.
The RADICALS-HD trial was initially presented at ESMO 2022 accruing 1,523 patients and randomizing them to no ADT vs 6 months of ADT, 6 months of ADT vs 24 months of ADT, or no ADT vs 6 months of ADT vs 24 months of ADT. At a median follow-up of 8.9 years, the 6 vs 24 month comparison showed an improvement in metastasis free survival, but no overall survival benefit: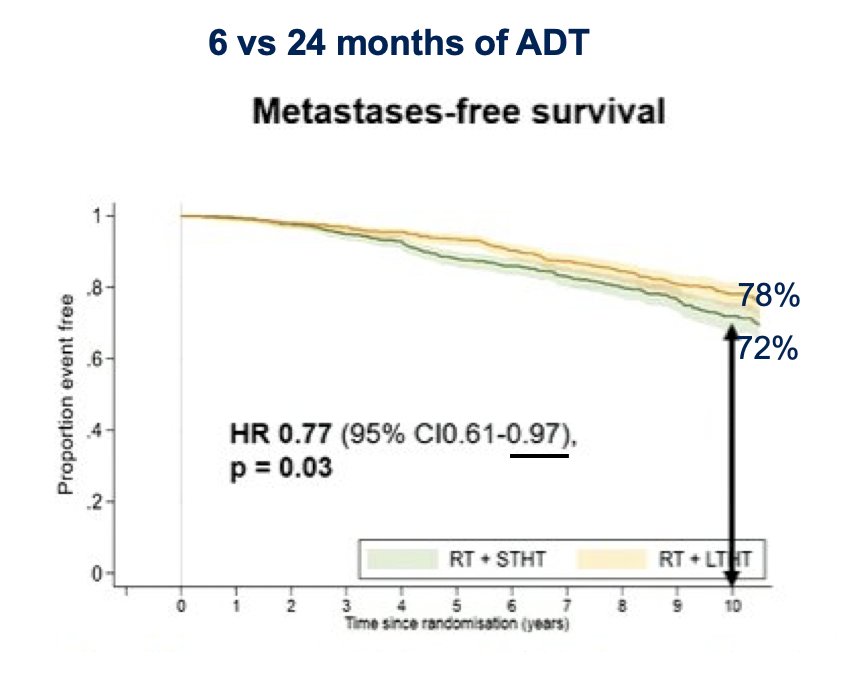
Dr. Dal Pra also discussed the FORMULA 509 trial, which compared salvage radiotherapy + 6 months of ADT vs salvage radiotherapy + 6 months of ADT + abiraterone/prednisone and apalutamide for 6 months. Patients had to have an unfavorable risk factor, including Gleason 8-10 disease, PSA > 0.5 ng/mL, pathologically positive nodes, pT3, or PSA doubling time < 10 months. Over a median follow-up of 34 months, there was no PFS benefit, thus this was a negative trial. However, in a preplanned subgroup analysis of patients treated with late salvage radiotherapy, there was a significant improvement in metastasis free survival (HR 0.32, 95% CI 0.13-0.84):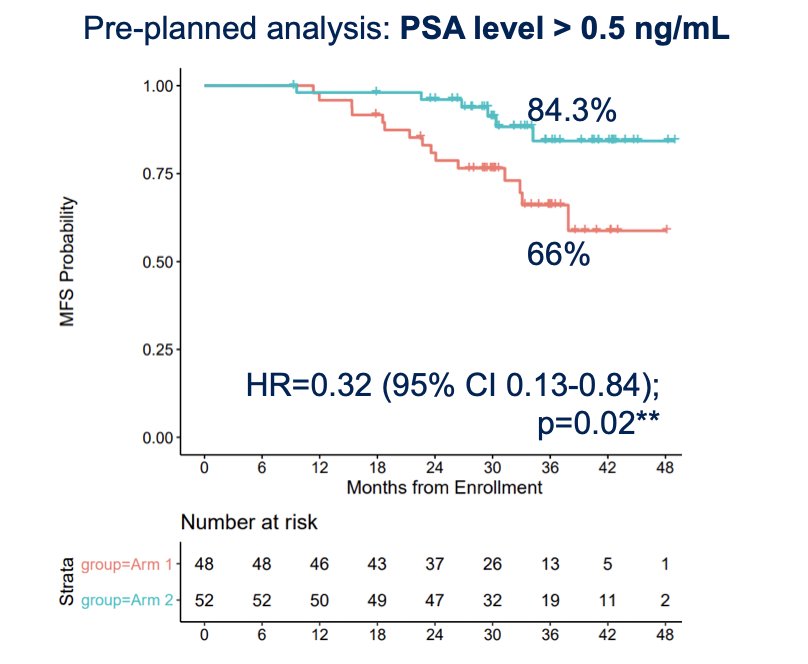
Dr. Dal Pra notes that this trial raises several interesting questions for patients with higher risk features, including the question whether we should be intensifying therapy for shorter duration instead of giving 24 months of ADT. This will be tested in the Prostate IQ trial.
Dr. Dal Pra then discussed the benefit of radiotherapy dose escalation. Although pre-clinical and retrospective data show radiotherapy dose response after prostatectomy, two randomized trials did not show any difference. The SAKK 09/10 trial, at a median follow-up of 6 years, showed no difference in freedom from biochemical progression when patients were randomized to 64 vs 70Gy, and a Chinese trial from Qi et al. also showed no benefit with dose escalation: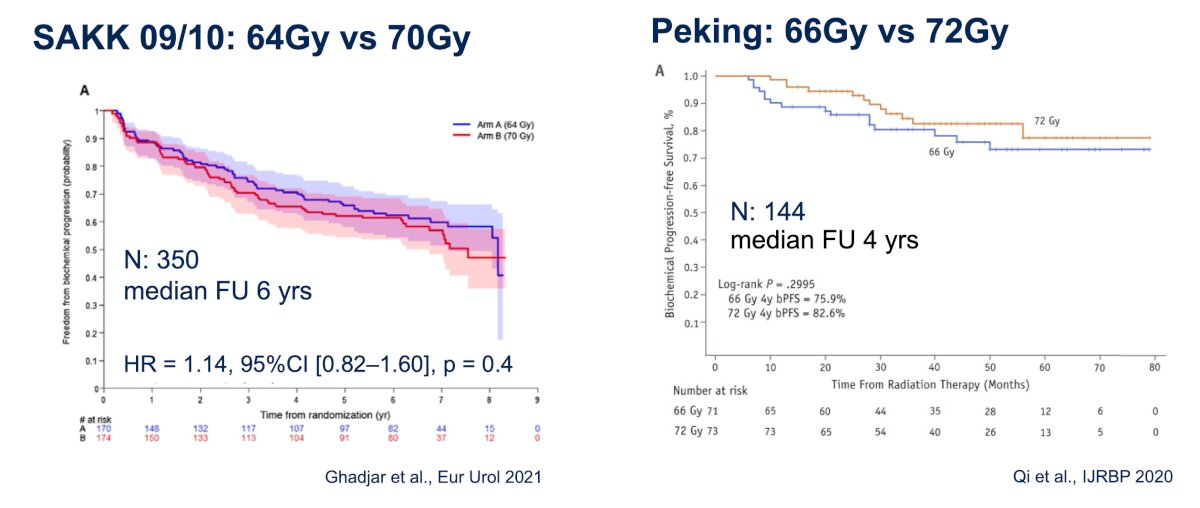
Should we use hypofractionation in the post-operative setting? To assess this question, the NRG GU 003 trial randomized 298 patients after prostatectomy to 66.6 Gy in 37 fractions (~7 weeks) vs 62.5 Gy in 25 fractions (5 weeks). The primary endpoint was a change in patient reported outcomes at two years, showing that a shorter course of treatment is associated with worse gastrointestinal scores at the end of radiotherapy, but with no difference at two years. However, the question is whether we need more follow up to confirm the safety and efficacy of hypofractionation in the postoperative setting. Referring again to the RADICALS-HD, this trial showed that early salvage is equivalent to adjuvant radiation. In RADICALS-HD, 34% of the patients were treated with hypofractionation using 52.5 Gy in 20 fractions (4 weeks of treatment only). At a median follow-up of 4.9 years, there were no differences in toxicity and quality of life. Importantly, this was an exploratory, nonrandomized comparison so results need to be understood in this context.
Dr. Dal Pra notes that over the past 10-15 years, radiation oncologists have followed prostate bed contouring guidelines mostly based on expert-consensus. Now, studies using novel imaging modalities have been able to map these recurrences more accurately and guide the development of new contouring guidelines not only for refinements in coverage but for better sparing of normal tissues. Moving further into treatment personalization, although there have been several RCTs published in the past few years, there are still important clinical questions when assessing patients after prostatectomy:
Prostate cancer biomarkers have been listed in national guidelines, in particular the NCCN guidelines. However, with regards to gene expression testing, Decipher is the only test considered to have level 1 evidence for validation according to the Simon's criteria. In a systemic review of 42 studies and 30,407 patients.6 Decipher was shown to be independently prognostic for biochemical failure, distant metastasis, prostate cancer specific mortality, and overall survival. In most studies, Decipher is more accurate in stratifying patient risk than clinicopathologic variables alone. Additionally, Decipher was validated in the SAKK 09/10 study for dose escalation, showing that a high Decipher score was associated with a 2-fold increased risk of progression (HR 2.1, 95% CI 1.3-3.3):7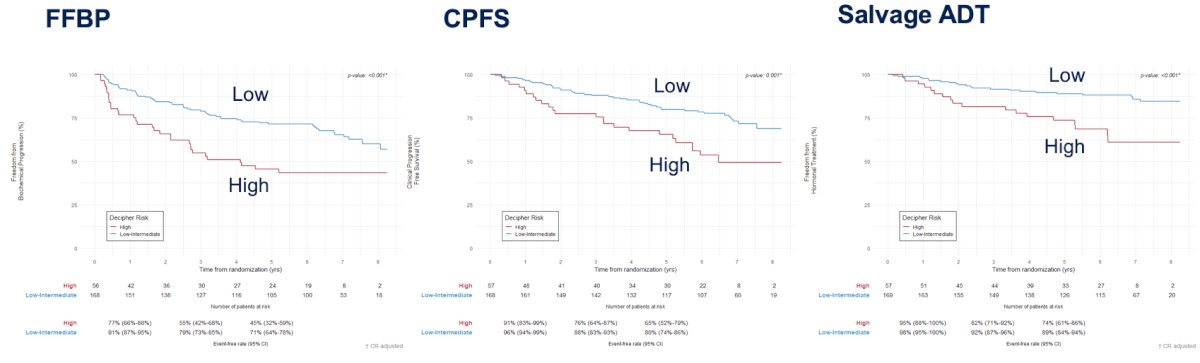
Can Decipher help guide the use of ADT? Feng et al. assessed tissue samples of the RTOG 9601 to address this question.8 This trial showed a much lower benefit of adding ADT in low Decipher patients. When the authors assessed the subgroup of patients treated at PSA < 0.7 ng/mL, there was very low predicted benefit in distant metastasis and prostate cancer specific mortality, but interestingly a detriment in overall survival:
Currently, there are two open trials for patients with biochemical recurrence. The first is the NRG-GU008 Innovate trial for patients with pathologic N+ disease and biochemical progression. Patients will be randomized to salvage radiotherapy and 2 years of ADT vs salvage radiotherapy + 2 years of ADT + apalutamide. The primary endpoint will be metastasis free survival: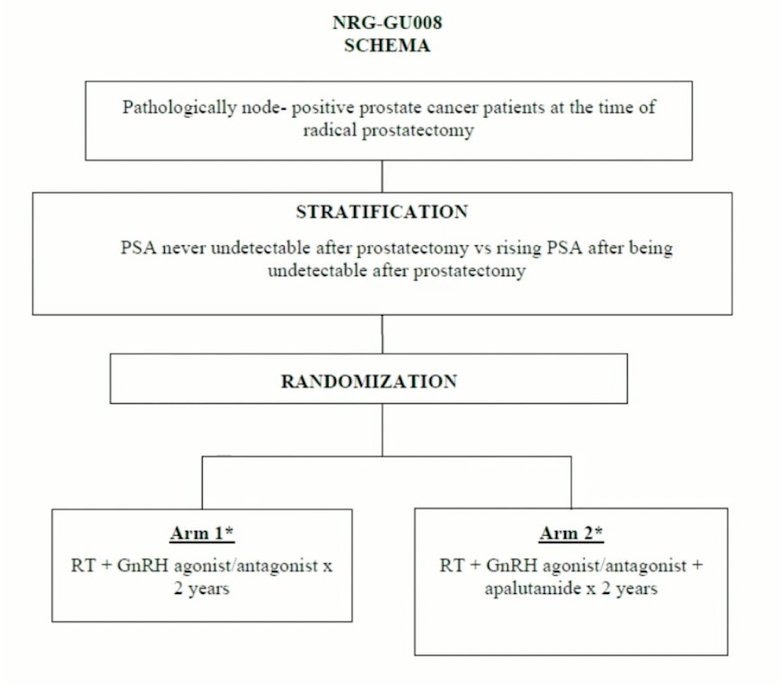
The second trial is the INDICATE trial that incorporates PSMA PET/CT into the treatment design for intensification with either enhanced systemic therapy or with metastasis-directed therapy: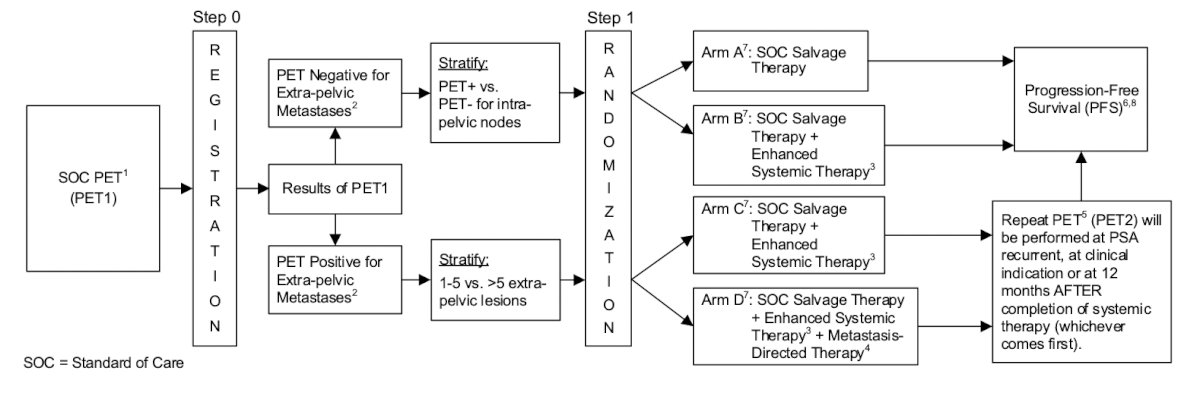
Dr. Dal Pra concluded this portion of this talk discussing salvage radiotherapy after prostatectomy with the following points:
- Salvage radiotherapy is the only potentially curative option for many patients
- Early salvage radiotherapy is associated with better outcomes
- A negative PSMA-PET should not preclude the use of early salvage radiotherapy if indicated
- Salvage radiotherapy with ADT improved outcomes, but may not be for everyone
- Dr. Dal Pra’s practice for these patients is as follows:
- It is reasonable to use salvage radiotherapy alone for patients with a PSA < 0.5 ng/mL, low-risk features, and low Decipher
- 6 months of ADT should be used for patients with PSA > 0.5 ng/mL or high-risk features (pT3b/4 and/or grade group ≥4 and/or high Decipher).
- Salvage radiotherapy + 2 years of ADT should be reserved for very select high-risk patients
- Elective pelvic nodal radiotherapy improves freedom from progression and time to second salvage ADT in the SPORT trial
- Although hypofractionation is evolving, conventional fractionation (~7 weeks) with doses not higher than 64-66 Gy is standard of care
- Biochemical recurrence after prostatectomy is a very heterogeneous state. We need trials incorporating predictive biomarkers not only for intensification but treatment de-intensification
Dr. Dal Pra then discussed salvage radiotherapy for local recurrence after radiotherapy. The natural history of biochemical recurrence after radiotherapy is highly variable, but overall, these patients have worse prognosis than biochemical recurrence after surgery. Even patients with an EAU low risk recurrence have a high cancer specific mortality, therefore appropriate treatment selection is key. When using PSMA PET/CT to stage these patients, a solitary intraprostatic local radio recurrence for PSA recurrence is common in ~33% of patients.
Local recurrence is important given that it is hypothesized that a first wave of distant metastasis stems from the emergence of occult micrometastatic disease that was present at the time of initial treatment, which may be followed by a subsequent second wave of distant metastasis representing “seeding” from a preceding local failure event. The workup for local recurrence includes PSMA PET/CT and mpMRI. Additionally, a biopsy is recommended, given that the irradiated prostate is the most common site of false positives on PSMA PET. Knowing when the right time to order a PSMA PET/CT is challenging given that several studies have shown high rates of positive PSMA PET/CT scans even in the absence of biochemical failure, however, the question is whether an intervention changes the clinical outcomes. Offering salvage local therapy has several advantages including an opportunity for cure and also avoiding the long-term effects of palliative systemic therapy: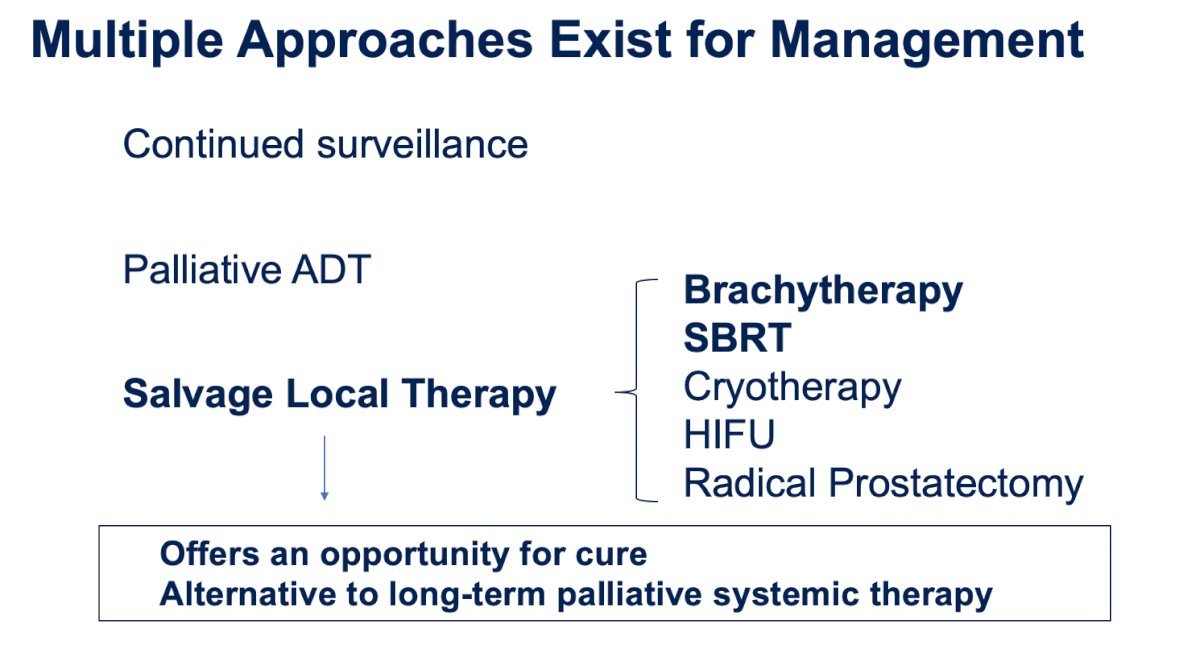
Dr. Dal Pra highlighted that the question regarding optimal salvage treatment in this setting was asked at the APCCC 2022 meeting, with the following quite balanced results: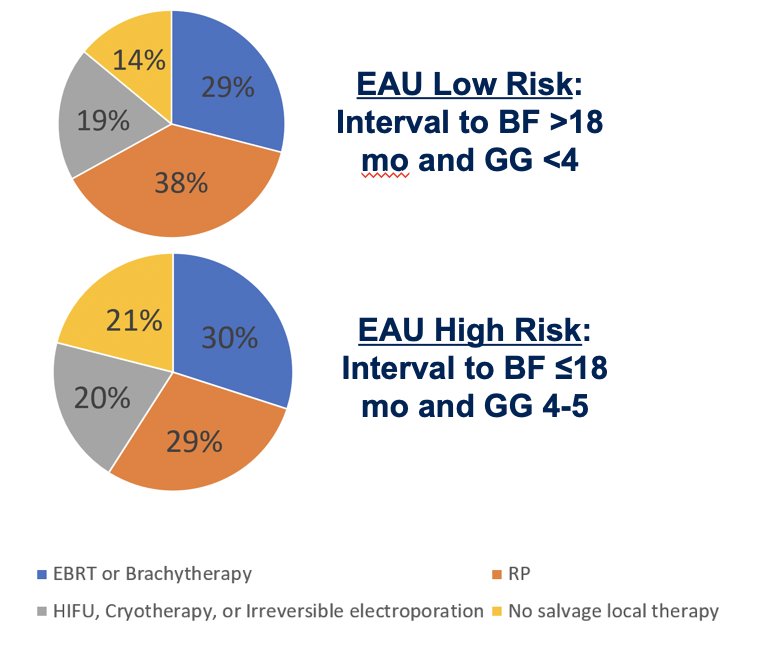
It is important to note that salvage re-irradiation is associated with severe toxicity risks, including grade 3 or higher GU toxicity of ~5-15% and grade 3 or higher GI toxicity of <5%. Several studies have shown that predictors of worse response to salvage re-irradiation include:
- Higher pre-salvage PSA level
- Shorter PSA doubling time
- Shorter disease-free interval
- ECE/SVI
- CRPC
There are several questions in the re-irradiation setting:
- Should we retreat locally in the setting of metastatic disease?
- What is the best form of salvage radiotherapy?
- Should we treat the entire gland vs whole gland therapy, which increases risk of complications?
- Should we combine radiation with ADT? What is the duration?
Dr. Dal Pra concluded this portion of his presentation discussing salvage radiotherapy options for biochemical recurrence after radiotherapy with the following take-home points:
- Local radio-recurrence is an increasingly identified disease state
- PSMA PET/CT, MRI, and biopsy are critical to identify and delineate the target
- Currently, there is no standard of care management approach
- Salvage brachytherapy and SBRT are safe and effective
- Because there are lots of unanswered questions, prospective trials are required to better define how to optimally select and treat patients with local recurrence after radiotherapy
Presented by: Alan Dal Pra, MD, University of Miami, Miami, FL
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the Genitourinary (GU) American Society of Clinical Oncology (ASCO) Annual Meeting, San Francisco, CA, Thurs, Jan 25 – Sat, Jan 27, 2024.
References:
- Tilki D, Chen MH, Wu J, et al. Prostate-Specific Antigen Level at the Time of Salvage Therapy After Radical Prostatectomy for Prostate Cancer and the Risk of Death. J Clin Oncol. 2023 May 1;41(13):2428-2435.
- Yokomizo A, Wakabayashi M, Satoh T, et al. Salvage Radiotherapy Versus Hormone Therapy for Prostate-specific Antigen Failure After Radical Prostatectomy: A Randomized, Multicentre, Open-label, Phase 3 Trial (JCOG0401). Eur Urol. 2020 Jun;77(6):689-698.
- Shipley WU, Seiferheld W, Lukka HR, et al. Radiation with or without Antiandrogen Therapy in Recurrent Prostate Cancer. N Engl J Med 2017;376(5):417-428.
- Carrie C, Hasbini A, de Laroche G, et al. Salvage radiotherapy with or without short-term hormone therapy for rising prostate-specific antigen concentration after radical prostatectomy (GETUG-AFU 16): A randomized, multicentre, open-label phase 3 trial. Lancet Oncol 2016;17(6):747-756.
- Pollack A, Karrison TG, Balogh AG, et al. The addition of androgen deprivation therapy and pelvic lymph node treatment to prostate bed salvage radiotherapy (NRG Oncology/RTOG 0534 SPPORT): An international, multicentre, randomized phase 3 trial. Lancet. 2022 May 14;399(10338):1886-1901.
- Jairath NK, Dal Pra A, Vince Jr. R, et al. A systematic review of the evidence for the Decipher Genomic Classifier in Prostate Cancer. Eur Urol. 2021 Mar;79(3):374-383.
- Dal Pra A, Ghadjar P, Hayoz S, et al. Validation of the Decipher genomic classifier in patients receiving salvage radiotherapy without hormone therapy after radical prostatectomy – An ancillary study of SAKK 09/10 randomized clinical trial. Ann Oncol. 2022 Sep;33(9):950-958.
- Feng FY, Huang HC, Spratt DE, et al. Validation of a 22-Gene Genomic Classifier in Patients with Recurrent Prostate Cancer: An Ancillary Study of the NRG/RTOG 9601 Randomized Clinical Trial. JAMA Oncol. 2021 Apr 1;7(4):544-552.


