(UroToday.com) The 2022 ASTRO annual meeting featured a prostate cancer session, including a presentation by Dr. Anjali Saripalli discussing using molecular imaging to create guidelines for the optimal clinical target volume for para-aortic lymph nodes. Molecular imaging enables improved understanding of the anatomic regions involved with metastatic prostate cancer due to the improved sensitivity compared to conventional imaging. Consequently, there is increasing awareness that prostate cancer metastasizes relatively frequently to the para-aortic lymph node region, compelling some radiation oncologists to electively cover this area if it is determined to be at high risk or if nodes are already involved. However, the optimal contouring boundaries are unknown. The objective of this study presented by Dr. Saripalli and colleagues is to use molecular imaging to develop guidelines for contouring the para-aortic clinical target volume in patients with prostate cancer.
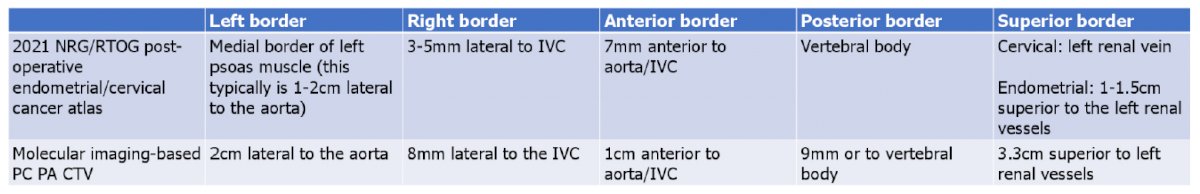
This study was a retrospective cohort study of patients with prostate cancer undergoing 18F-fluciclovine or 18F-DCFPyL PSMA PET/CT at a single institution. Images of patients with PET-positive para-aortic lymph node involvement were imported into the treatment planning system and the avid nodes were contoured. The radial distance from the epicenter of each node was measured in all dimensions relative to the inferior vena cava and aorta, and superiorly relative to the left renal vein. The para-aortic clinical target volume was delineated per the 2021 NRG/RTOG post-operative endometrial/cervical cancer atlas, as principles of these malignancies are frequently used to delineate this region. Descriptive statistics were used to assess the performance of this gynecologic atlas and generate recommendations for contouring in prostate cancer patients.
There were 246 men that had molecular PET imaging from October 2016 to January 2022 (48% 18F-fluciclovine, 52% PSMA). Overall, 31 men (13%) had evidence of para-aortic nodal metastasis. In these patients, 16% had de novo, 52% recurrent, and 32% castration-resistant metastatic prostate cancer. The median number of positive para-aortic lymph nodes per patient was 1 (IQR 1-3.5). The distance from central vasculature and left renal vein are as follows:
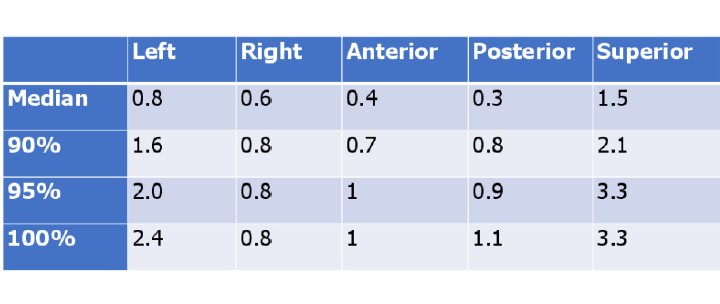
Only 66% of para-aortic nodes were covered using the left renal vein as the superior border and 75% were covered using 1.5 cm above the left renal vein. Overall, the gynecologic atlas missed 25% of nodes (57% due to left sided and 30% due to superior misses), suggesting unique target delineation should be considered for prostate cancer patients. As follows are the recommendations for expanding the prostate cancer para-aortic clinical target volume in the left lateral and superior dimensions:
Dr. Saripalli concluded this presentation discussing using molecular imaging to create guidelines for the optimal clinical target volume for para-aortic lymph nodes with the following take home messages:
- This study used molecular PET imaging to determine the anatomic patterns of para-aortic metastasis to develop contouring guidelines for creating a para-aortic clinical target volume in patients with prostate cancer
- Although the optimal patient selection and clinical benefits of para-aortic radiotherapy remain uncertain, these results will aid in delineating the optimal target and are currently being validated in an independent dataset
Presented by: Anjali Saripalli, Loyola University Chicago, Loyola University Medical Center and Edward Hines Jr., VA Hospital, Stritch School of Medicine, Department of Radiation Oncology, Cardinal Bernardin Cancer Center, Maywood, IL
Co-Authors: N. Bhandare2, B. Venkatesulu1, G. Harmon1, A. M. Block1, W. Small Jr3, J. S. Welsh1, M. M. Harkenrider1, and A. A. Solanki1; 1Loyola University Chicago, Loyola University Medical Center and Edward Hines Jr., VA Hospital, Stritch School of Medicine, Department of Radiation Oncology, Cardinal Bernardin Cancer Center, Maywood, IL, 2Department of Radiation Oncology, Edward Hines VA Hospital, Maywood, IL, 3Loyola University Chicago, Loyola University Medical Center, Stritch School of Medicine, Department of Radiation Oncology, Cardinal Bernardin Cancer Center, Maywood, IL
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Radiation Oncology (ASTRO) Annual Hybrid Meeting, San Antonio, TX, Sat, Oct 22 – Wed, Oct 26, 2022.


