(UroToday.com) The 2022 ASTRO annual meeting featured a prostate cancer session, including a presentation by Dr. Rebecca Krc discussing a secondary analysis of RTOG 0126 and RTOG 0415, specifically a toxicity analysis of patients with prostate cancer treated with 3D-conformal radiotherapy (3D-CRT) compared to intensity-modulated radiotherapy (IMRT). Patients with low- and intermediate-risk prostate cancer have excellent control rates following definitive radiation therapy, but may experience treatment morbidity that impacts quality-of-life. To decrease normal tissue toxicity, modern techniques such as IMRT have largely replaced 3D-CRT for prostate cancer. The objective of our study was to describe the comparative benefit of IMRT over 3D-CRT for patients undergoing prostate radiation therapy across different radiation therapy dosing and fractionation schemes.
This study was a post-hoc analysis of patients enrolled on RTOG 0126 and RTOG 0415. RTOG 0126 randomized to dose escalated, conventionally fractionated radiation therapy (79.2 Gy in 44 fractions) or standard dose conventionally fractionated radiation therapy (70.2 Gy in 39 fractions). RTOG 0415 randomized to hypofractionated radiation therapy (70 Gy in 28 fractions) or standard dose conventionally fractionated radiation therapy (73.8 Gy in 41 fractions). Treatment with 3D-CRT and IMRT was at the discretion of the treating physician; target organ at risk dose constraints were the same irrespective of radiation therapy modality. Dr. Krc and colleagues performed a logistic regression analysis of radiation therapy modality and acute and late grade 2+ gastrointestinal or genitourinary toxicity as per CTCAE criteria across the different dose regimens.
A total of 2,590 patients treated in both studies were included in this analysis. The median patient age was 69 and median follow up was 6.9 years. On RTOG 0126, 66.3% and 33.7% were treated with 3DCRT and IMRT respectively, while 20.6% and 78.2% were treated with 3D-CRT and IMRT on RTOG 0415, respectively. The patient characteristics of each study arm are as follows:
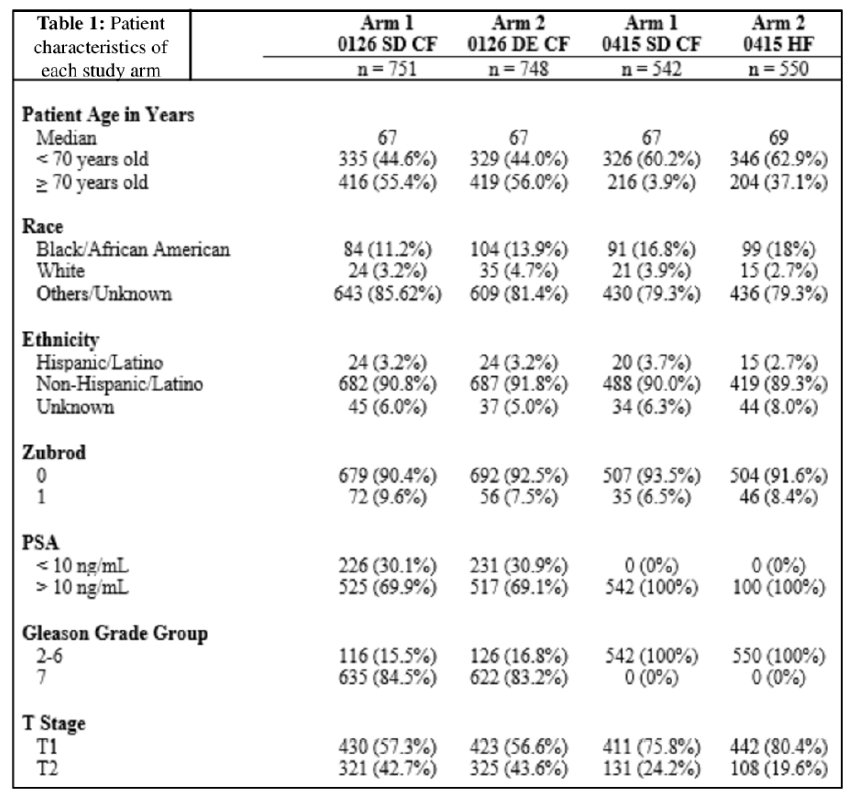
On both studies combined, the overall rate of acute grade 2+ gastrointestinal and genitourinary toxicity was 7.7% and 20.9%, respectively; the rate of late grade 2+ gastrointestinal and genitourinary toxicity was 18.2% and 17.5%, respectively. There was no significant difference in acute grade 2+ gastrointestinal or genitourinary toxicity between those treated with either radiation therapy modality across the different dosing regimens. For patients receiving dose escalated conventionally fractionated radiation therapy, IMRT resulted in improved late grade 2+ gastrointestinal toxicity compared to 3D-CRT (16.8% vs. 23.4%, OR 0.65, 95% CI 0.44-0.96, p = 0.03). There was also a significant improvement in late grade 2+ genitourinary toxicity with the use of IMRT compared to 3D-CRT (9.4% vs. 16.1%, OR 0.53, 95% CI 0.32-0.86, p = 0.01). However, there was no significant difference in toxicity rates between IMRT and 3D-CRT for late gastrointestinal or genitourinary toxicity when using standard dose conventionally fractionated radiation therapy or hypofractionated radiation therapy:
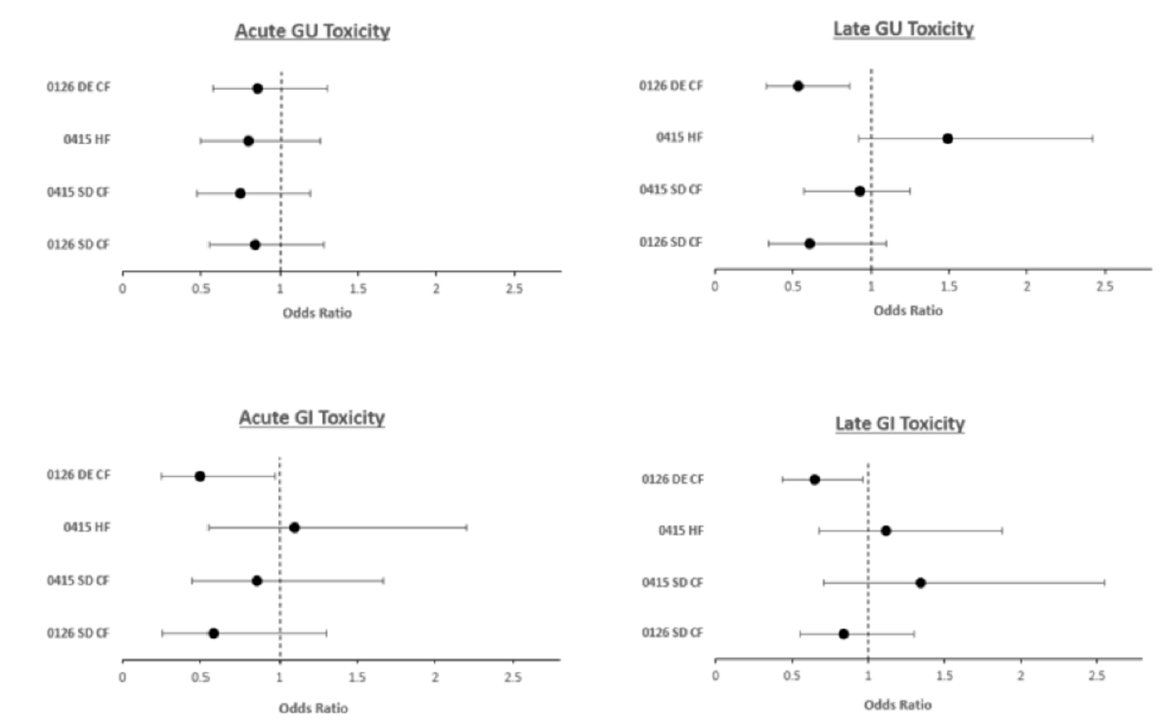
Dr. Krc concluded her presentation by discussing a toxicity analysis of patients with prostate cancer treated with 3D-CRT compared to IMRT with the following concluding messages:
- Patients undergoing conventionally fractionated dose-escalated radiotherapy benefit from IMRT, while patients receiving conventionally fractionated standard dose (70.2Gy or 73.8 Gy) radiation therapy or hypofractionated radiation therapy did not show a difference in toxicity based on radiation therapy modality
- These data provide a framework to compare the relative benefit of modern radiation therapy techniques (e.g., proton, SBRT, MR-guided radiation therapy) to IMRT in future studies
Presented by: Rebecca F. Krc, DO, Department of Radiation Oncology, University of Maryland Medical Center, Baltimore, MD
Co-Authors: J. W. Assif2, G. S. Alexander1, K. Sun3, J. K. Molitoris4, Z. H. Rana2, P. T. Tran2, S. M. Bentzen3, and M. V. Mishra2; 1Department of Radiation Oncology, University of Maryland Medical Center, Baltimore, MD, 2Department of Radiation Oncology, University of Maryland School of Medicine, Baltimore, MD, 3Division of Biostatistics and Bioinformatics, University of Maryland Greenebaum Cancer Center, and Department of Epidemiology and Public Health, University of Maryland School of Medicine, Baltimore, MD, 4University of Maryland School of Medicine, Baltimore, MD
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Radiation Oncology (ASTRO) Annual Hybrid Meeting, San Antonio, TX, Sat, Oct 22 – Wed, Oct 26, 2022.


