(UroToday.com) The 2022 ASTRO annual meeting featured a prostate cancer session, including a presentation by Dr. Dylan Conroy discussing a correlation between obesity and treatment failure following stereotactic body radiation therapy for clinically localized prostate cancer. Cancer control outcomes are significantly worse in obese prostate cancer patients. Over the past decade, stereotactic body radiation therapy has been established as a safe and effective treatment for localized prostate cancer. Accurate delivery of external beam radiation could be adversely affected by increased pelvic adipose tissue and result in worse biochemical control. However, data reporting on the efficacy of stereotactic body radiation therapy stratified by BMI is limited. This single-institution study by Dr. Conroy and colleagues sought to evaluate oncologic outcomes following stereotactic body radiation therapy for prostate cancer in men based on BMI.
This was a retrospective chart review performed on all patients with localized prostate cancer treated with stereotactic body radiation therapy at a single institution between 2006 to 2021. Treatment was delivered using robotic stereotactic body radiation therapy with doses of 35-36.25 Gy in 5 fractions, per institutional protocol. Biochemical recurrence was defined by the Phoenix definition (PSA rise ≥ 2 ng/mL above nadir). Multiple regression Cox proportional hazard analysis was performed.
There were 1,306 patients identified, with a mean follow-up of 47 months. The patients were elderly (median age = 70 years) and overweight (median BMI = 27.6 kg/m2), and the majority were low to intermediate risk (88%) according to the D’Amico classification. The median pre-treatment PSA was 7.4 ng/mL, 23.7% received neoadjuvant ADT, and BMI (kg/m2) was calculated prior to initiation of treatment and patients were stratified as: BMI < 25, 25 – 29.9, 30 – 34.9, ≥ 35. The complete baseline characteristics are as follows:
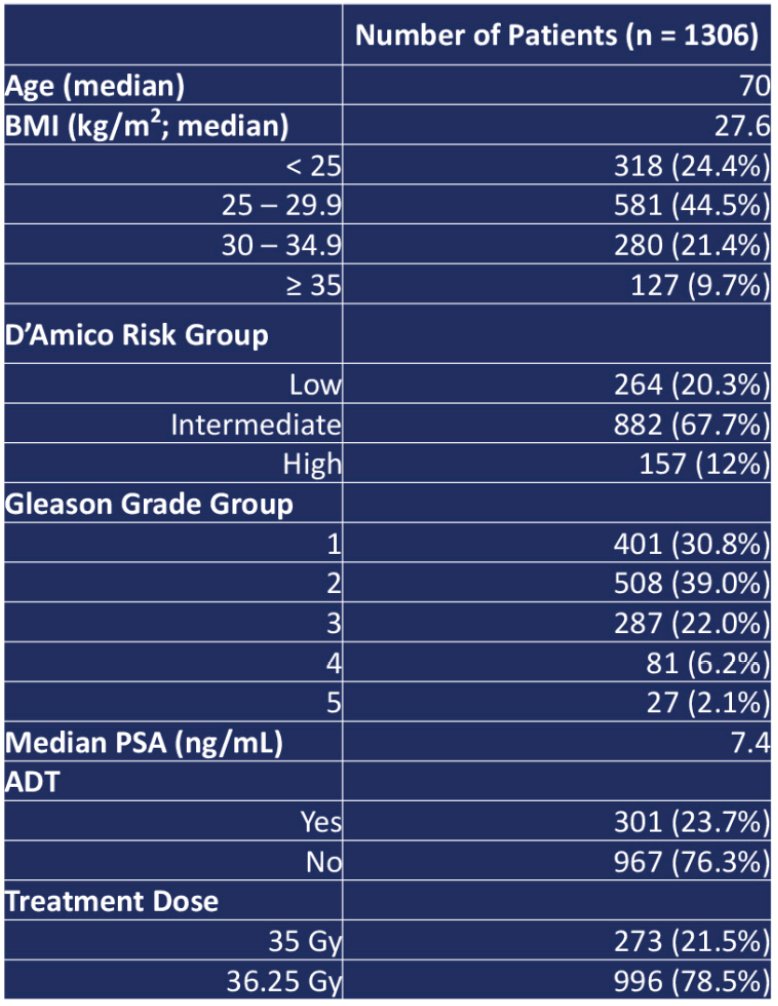
There was no statistically significant difference between pre-treatment PSA or Gleason’s score between BMI groups. A multiple regression Cox proportional hazard analysis was performed, with BMI < 25 set as the reference, finding no statistically significant difference in biochemical disease-free survival, distant metastasis-free survival, or disease-specific survival between BMI subgroups. The Kaplan Meier analysis between BMI and biochemical disease-free survival is as follows:

The Kaplan Meier analysis between BMI and distant metastasis free survival is as follows:
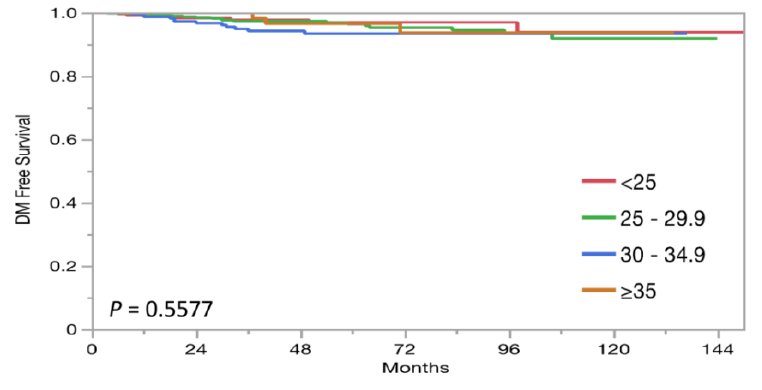
Dr. Conroy concluded his presentation discussing a correlation between obesity and treatment failure following stereotactic body radiation therapy for clinically localized prostate cancer with the following take home messages:
- In the general population, cancer control following prostate stereotactic body radiation therapy is equivalent to other standard radiation options
- In this analysis, increased BMI did not portend worse oncologic outcomes following stereotactic body radiation therapy when analyzing biochemical disease-free survival, distant metastasis-free survival, or disease-specific survival
- Therefore, obesity should not be considered a contraindication to prostate stereotactic body radiation therapy
Presented by: Dylan Conroy, MD, Department of Radiation Medicine, Medstar Georgetown University Hospital, Washington, DC
Co-Authors: T. Sholklapper2, M. K. K. Lawlor2, J. M. Cantalino3, A. Zwart4, M. J. Ayoob4, M. Danner1, T. Yung4, B. T. Collins1, S. Lei4, A. Rashid4, D. Kumar5, S. Suy1, N. Aghdam6, and S. P. Collins1; 1Department of Radiation Medicine, Medstar Georgetown University Hospital, Washington, DC, 2Georgetown University School of Medicine, Washington, DC, 3Brigham and Women's Hospital, Boston, MA, 4Department of Radiation Medicine, MedStar Georgetown University Hospital, Washington, DC, 5Biotechnology Research Institute, North Carolina Central University, Durham, NC, 6Department of Radiation Medicine, Georgetown University Hospital, Washington, DC
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Radiation Oncology (ASTRO) Annual Hybrid Meeting, San Antonio, TX, Sat, Oct 22 – Wed, Oct 26, 2022.


