(UroToday.com) The 2022 ASTRO annual meeting featured a prostate cancer session, including a presentation by Dr. Simon Spohn discussing the maximum standardized uptake value in patients with recurrent or persistent prostate cancer after radical prostatectomy and PSMA-PET-guided salvage radiotherapy. Up to 50% of patients with localized prostate cancer undergoing radical prostatectomy experience biochemical relapse within the first 5 years after treatment. Recurrence rate after salvage radiotherapy is heterogeneous and additional prognostic markers are needed to improve risk-stratification and guide personalized treatment. Dr. Spohn and colleagues evaluated the association of the maximum standardized uptake value (SUVmax) in positron-emission tomography targeting prostate-specific-membrane-antigen (PSMA-PET) prior to salvage radiotherapy on biochemical recurrence free survival in a large multicenter cohort.
Patients who underwent 68Ga-PSMA11-PET after radical prostatectomy due to biochemical recurrence or PSA-persistence were enrolled in four high-volume centers in this retrospective multicenter study. Only patients with PET-positive local recurrence and/or nodal recurrence within the pelvis were included. Patients were treated with intensity-modulated-salvage radiotherapy to the prostatic fossa and elective lymphatics in case of nodal disease. Dose escalation was delivered to PET-positive local recurrence and nodal recurrence. Androgen deprivation therapy was administered at the discretion of the treating physician. Local recurrence and nodal recurrence were manually delineated and SUVmax was extracted for local recurrence and nodal recurrence. Cox-regression was performed to analyze the impact of clinical parameters and the SUVmax-derived values on biochemical recurrence free survival, defined as serum PSA >0.2 ng/ml above the post-salvage radiotherapy-nadir without initiation of additional salvage therapies or death of any cause.
There were 235 patients with a median follow up of 24 months (197 patients with > 12 months of follow-up) included in the final cohort. As follows is the baseline patient characteristics of this cohort:
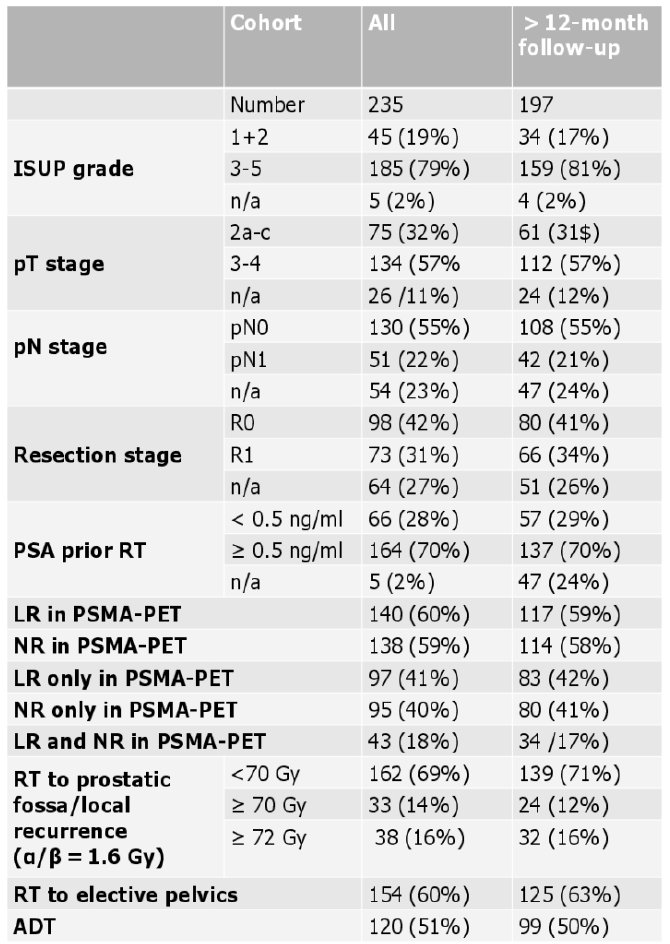
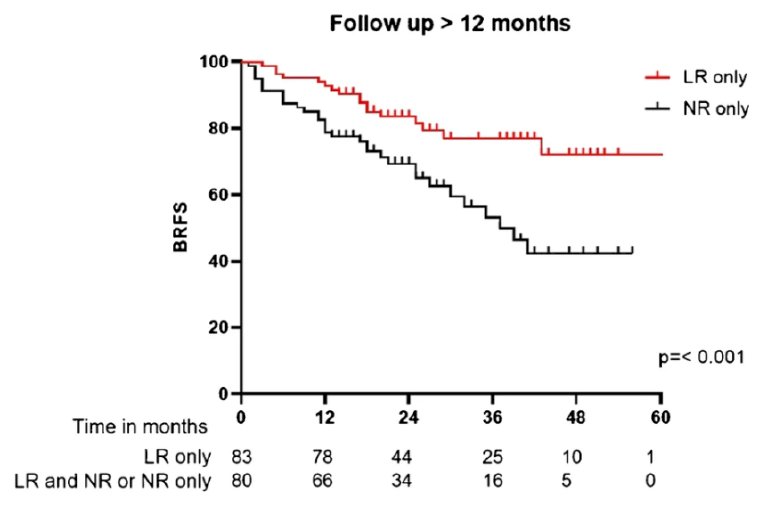
The presence of local recurrence was associated with favorable biochemical recurrence free survival (p = 0.016). Presence of nodal recurrence was associated with unfavorable biochemical recurrence free survival (p = 0.007). As follows is the Kaplan-Meier curve for biochemical recurrence free survival for patients with local recurrence only and nodal recurrence only:
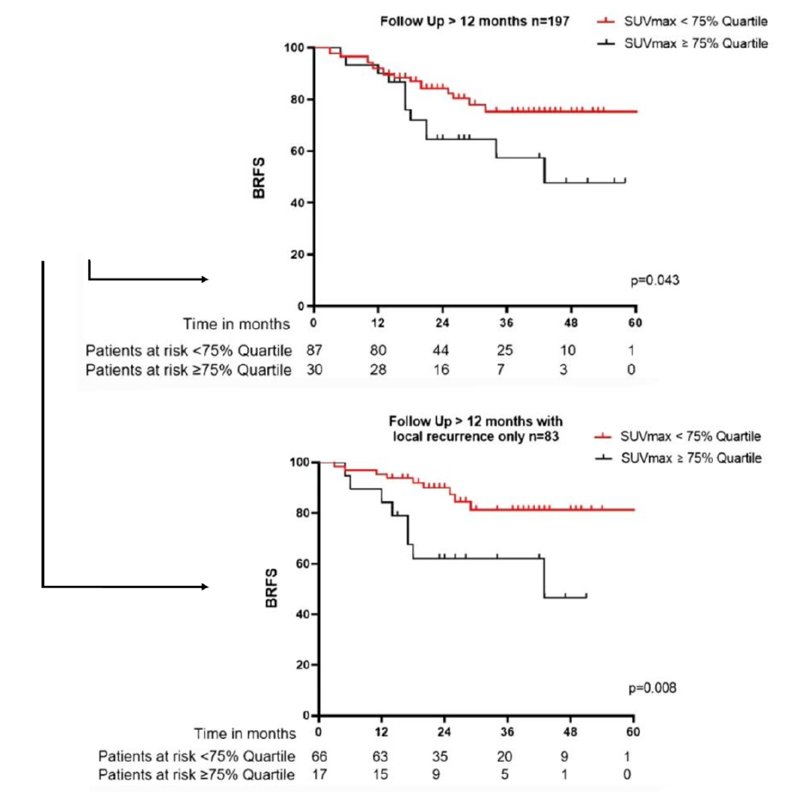
While there was a trend for SUVmax values ≥ median (p = 0.071), SUVmax values ≥ 75% quartile in local recurrence were significantly associated with unfavorable biochemical recurrence free survival (p = 0.022, HR: 2.1, 95% CI 1.1-4.6). SUVmax value in nodal recurrence was not significantly associated with biochemical recurrence free survival. Furthermore, SUVmax in local recurrence stayed significant in multivariate analysis (p = 0.030). A sensitivity analysis with patients for who had a follow up of >12 months confirmed these results:
Dr. Spohn concluded his presentation discussing the maximum standardized uptake value in patients with recurrent or persistent prostate cancer after radical prostatectomy and PSMA-PET-guided salvage radiotherapy with the following take home messages:
- In patients with biochemical recurrence/persistence after radical prostatectomy, presence of PSMA-expressing pelvic lymph nodes on PET is associated with less favorable biochemical recurrence free survival after salvage-radiotherapy
- The non-invasive biomarker SUVmax can prognosticate outcome in patients undergoing salvage radiotherapy and recurrence confined to the prostatic fossa in PSMA-PET
Presented by: Simon K. B. Spohn, MD, Department of Radiation Oncology, University Medical Center Freiburg, Freiburg, Germany
Co-Authors: A. Farolfi2, S. Schandeler1, M. M. Vogel3, J. Ruf4, M. Mix4, S. Kirste1, F. Ceci5, S. Fanti2, H. Lanzafame2, C. Gratzke6, A. Sigle6, S. E. Combs3, D. Bernhardt3, J. E. Gschwend7, J. A. Buchner3, C. Trapp8, C. Belka8, P. Bartenstein9, M. Eiber10, S. Nekolla10, K. Schiller3, A. Grosu1, N. S. Schmidt-Hegemann8, C. Zamboglou1, and J. C. Peeken3; 1Department of Radiation Oncology, University Medical Center Freiburg, Freiburg, Germany, 2Service of Nuclear Medicine, S.Orsola Hospital, University of Bologna, Bologna, Italy, 3Department of Radiation Oncology, Technical University of Munich (TUM), Munich, Germany, 4Department of Nuclear Medicine, University Medical Center Freiburg, Freiburg, Germany, 5Division of Nuclear Medicine, IEO European Institute of Oncology Scientific IRCCS, Milan, Italy, 6Department of Urology, University Medical Center Freiburg, Faculty of Medicine, Freiburg, Germany, 7Department of Urology, Klinikum rechts der Isar, Technical University of Munich, Munich, Germany, 8Department of Radiation Oncology, University Hospital, Ludwigs-Maximials Universität (LMU), Munich, Germany, 9Department of Nuclear Medicine, University Hospital, Ludwigs-Maximials Universität (LMU), Munich, Germany, 10Department of Nuclear Medicine, Klinikum rechts der Isar, Technical University of Munich, Munich, Germany
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Radiation Oncology (ASTRO) Annual Hybrid Meeting, San Antonio, TX, Sat, Oct 22 – Wed, Oct 26, 2022.


