(UroToday.com) The 2022 ASTRO annual meeting featured a prostate cancer session, including a presentation by Dr. Krystal Morales Rivera discussing patterns of care after 68Ga-PSMA-PET (PSMA) in patients with radio recurrent localized only prostate cancer. The utilization of molecular imaging in men with recurrent prostate cancer after definitive treatment is rapidly increasing. However, randomized data to guide preferred treatment approaches after molecular imaging are lacking, particularly for men with radiorecurrent, localized-only disease. Dr. Morales Rivera and colleagues sought to evaluate patterns of care in these men, in order to understand the referral patterns and care plans implemented as a result of molecular imaging.
From 2018-2020, 825 men were enrolled at a single institution on a prospective study (NCT03396874) assessing the diagnostic performance of (PSMA) in men with biochemical recurrence after initial definitive therapy. Among the 199 (24%) men treated with upfront definitive radiation therapy, 58 had an isolated local recurrence and form the cohort for the present analysis. Dr. Morales Rivera and colleagues evaluated the patterns of care including the specialty of ordering provider, patterns of consulted specialties after PSMA, and subsequent management.
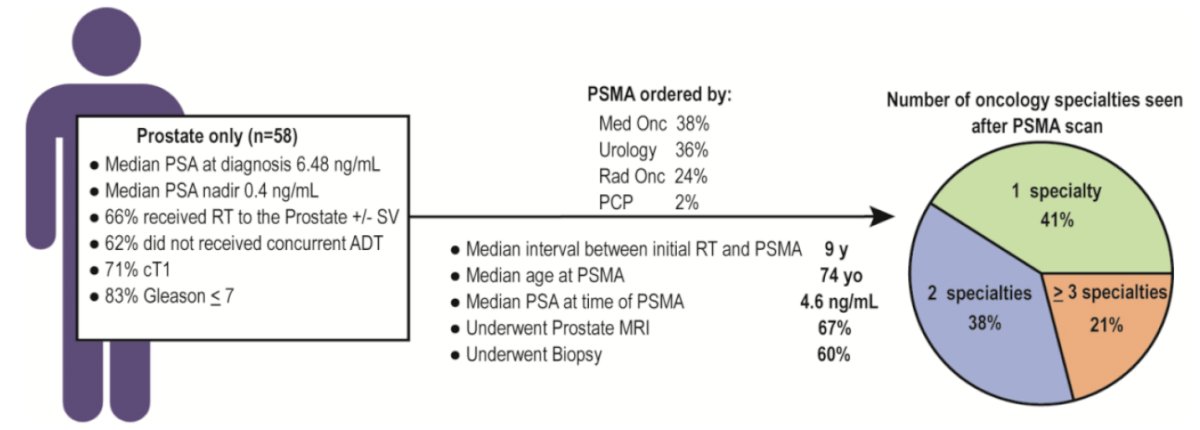
Fifty-eight men had PSMA-positive radio recurrent localized-only disease (29%). PSMA for these men was most ordered by medical oncology (38%), urology (36%), and radiation oncology (24%). Median PSA at time of PSMA was 4.6 ng/mL, and the median interval between initial radiation therapy and PSMA was 9 years. After PSMA, 101 consultations were completed, 40 by urology (40%), 33 by radiation oncology (32%), and 28 by medical oncology (28%). Twenty-one percent of men saw all three specialties, 38% two specialities, and 41% one specialty. Sixty-seven percent of men underwent prostate MRI and 60% had a prostate biopsy:
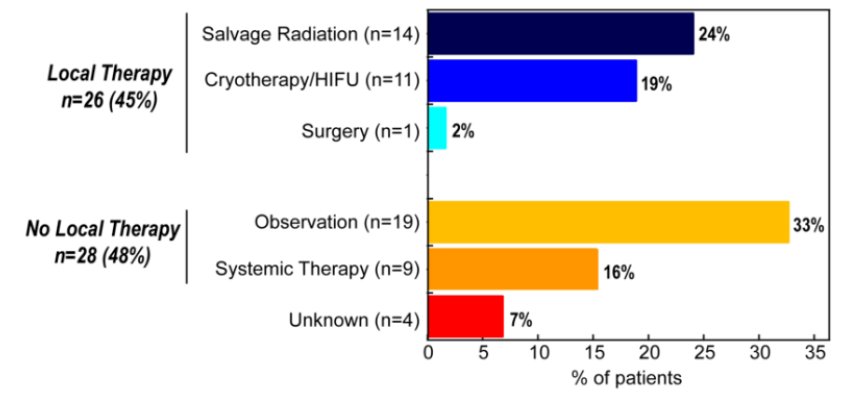
In total, 26 men (45%) underwent local therapy, which included salvage radiation therapy in 14 men (24%) [brachytherapy (n=9), SBRT (n=5)], cryotherapy/HIFU in 11 men (19%), and salvage prostatectomy for one (2%). Among the 28 patients (48%) not undergoing local therapy, 16% (n=9) were poor local therapy candidates due to poor GU/GI quality of life or prior focal therapy and received systemic therapy alone. Approximately one-third of patients underwent observation (n=19), driven frequently by patient preference rather than local therapy eligibility or age-related comorbidities (n=12/19, 63%):
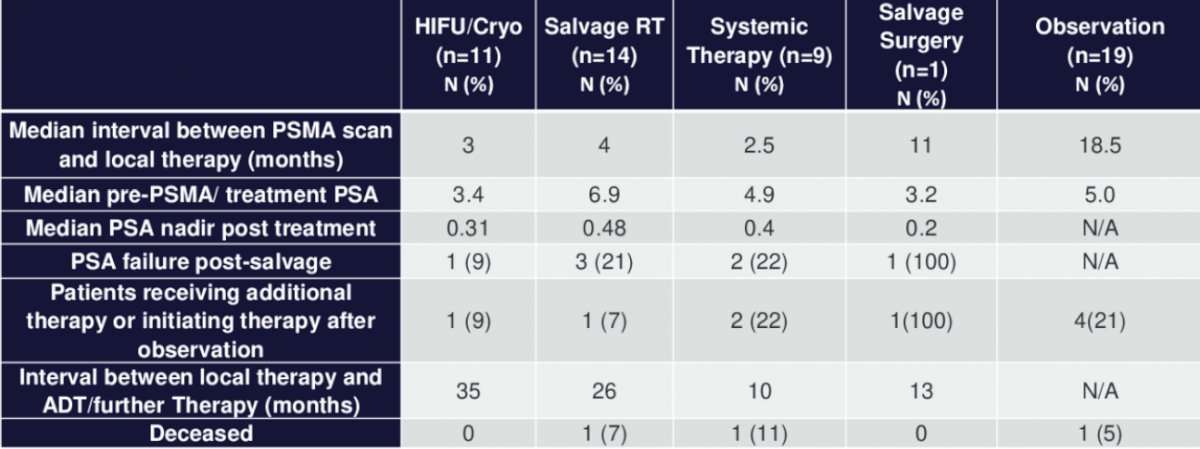
At a median follow-up of 23 months after PSMA, only 3 men (11.5%) who received local therapy and 6 (21%) out of the cohort who did not receive local therapy required initiation of additional treatment:
Dr. Morales Rivera concluded her presentation discussing patterns of care after 68Ga-PSMA-PET in patients with radiorecurrent localized only prostate cancer with the following concluding messages:
- This data demonstrate significant heterogeneity in the management of patients with PSMA radiorecurrent localized-only prostate cancer
- As molecular imaging becomes more ubiquitous, this data demonstrates the need for multidisciplinary discussion as well as randomized trials in these patients to help guide the optimal treatment approach for this population
Presented by: Krystal A. Morales Rivera, MD, PhD, Department of Radiation Oncology, University of Michigan, Ann Arbor, MI
Co-Authors: I. Tsung2, C. Mayo1, M. Piert3, B. L. Viglianti4, K. D. Stensland5, A. George5, J. Montgomery5, T. M. Morgan5, S. Kaffenberger5, L. Herrel6, S. E. Yentz6, M. E. Caram6, J. Alumkal6, P. Palmbos5, Z. Reichert7, D. E. Spratt8, R. T. Dess1, and W. C. Jackson1; 1Department of Radiation Oncology, University of Michigan, Ann Arbor, MI, 2Department of Internal Medicine, Division of Medical Oncology, University of Michigan, Ann Arbor, MI, 3Department of Radiology, University of Michigan, Ann Arbor, MI, 4Department of Radiology, Nuclear Medicine Service, University of Michigan, Ann Arbor, MI, 5Department of Urology, University of Michigan, Ann Arbor, MI, 6University of Michigan, Ann Arbor, MI, 7Department of Medical Oncology, University of Michigan, Ann Arbor, MI, 8University Hospitals Seidman Cancer Center, Case Western Reserve University, Cleveland, OH
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Radiation Oncology (ASTRO) Annual Hybrid Meeting, San Antonio, TX, Sat, Oct 22 – Wed, Oct 26, 2022.


