(UroToday.com) The 2022 ASTRO annual meeting featured a session on bladder and kidney preservation, including a presentation by Dr. Martin Swinton discussing clinical outcomes in cN+M0 bladder cancer patients. Optimal management of patients initially presenting with clinically node positive non-metastatic (cN+M0) bladder cancer is a topic of debate with significant variation in practice worldwide. In the UK, fit patients are offered – after platinum-based chemotherapy - either radical cystectomy or radical radiotherapy – a bladder preserving treatment. However, there is a paucity of evidence to guide clinician and patient decision making on choice of treatment. As such, Dr. Swinton and colleagues undertook a multi-center UK retrospective analysis to assess clinical outcomes for cN+M0 bladder cancer.
A multicenter retrospective analysis was conducted on patients from four large UK oncology centers. Patients initially presenting with cN+M0 bladder cancer between 2012 and 2021 were identified, and data was collected on treatment received, clinical outcomes and patient and tumor factors. Overall survival (OS) was calculated as time from initial diagnosis of bladder cancer. Univariable and multivariable analysis was performed on patients receiving radical treatment using the variables: age, performance status, T and N stage, primary chemotherapy, and radical treatment received.
There were 288 of 292 patients with cN+M0 bladder cancer identified that had survival data available for analysis, of which 165 of 288 patients received a treatment with radical intent:
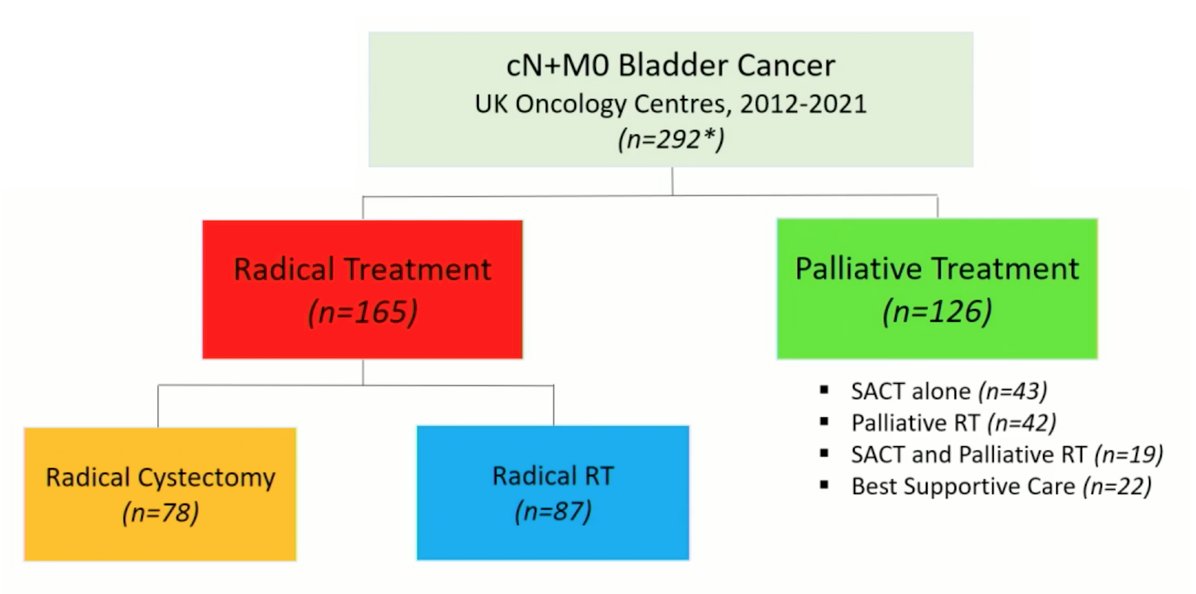
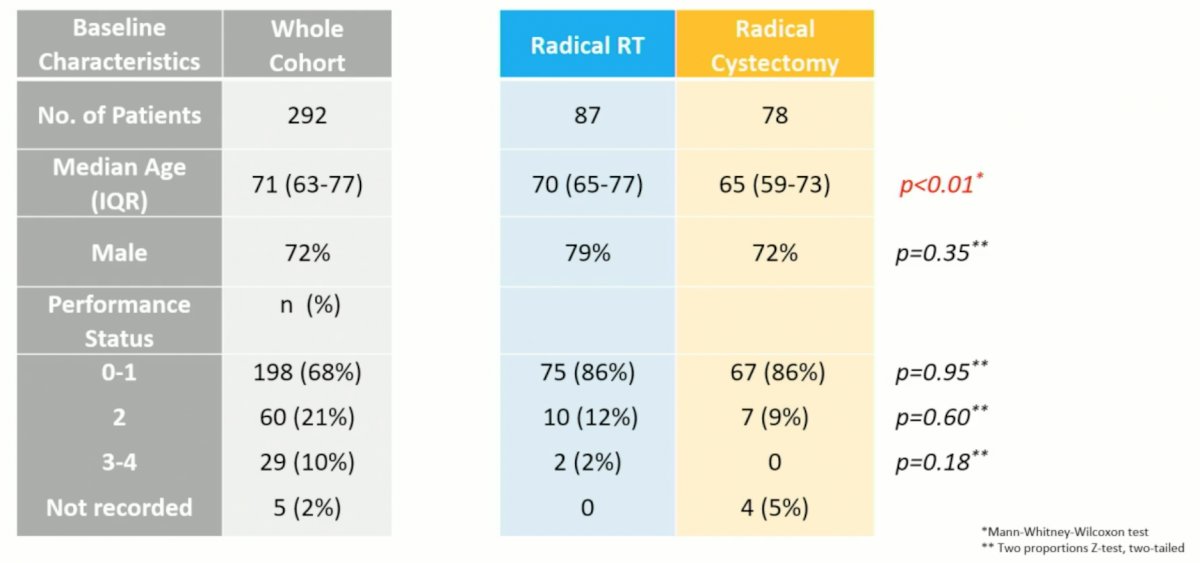
There were 87 patients that had radical radiotherapy and 78 patients that had radical cystectomy among the 165 patients receiving radical treatment. There were few differences between the two groups, except for patients undergoing radical cystectomy being young (median 65 years vs 70 years; p < 0.01):
Patients that underwent radical radiotherapy had greater use of primary chemotherapy, whereas those undergoing radical cystectomy had greater use of adjuvant chemotherapy:

The radiotherapy details for this cohort of patients is as follows:

The median OS of the whole analyzed cohort (n = 288) was 1.54 years (95% CI 1.35-1.82).
OS was significantly higher in the radical vs palliative treatment group (log-rank test, p < 0.0001), with the median OS in the radical and palliative groups being 2.4 years (95% CI 1.9-2.7) and 0.89 years (95% CI 0.67-1.1), respectively:

Patients treated radically received either radical cystectomy (n = 76) or radical radiotherapy (n = 87) with no difference in OS between the two groups (log-rank test p = 0.47). The median OS for those receiving radical radiotherapy was 2.53 years (95% CI 2.02 -3.44) versus 2.09 years (95% CI, 1.79-3.13) for radical cystectomy:

In a univariable analysis of patients receiving radical treatment, improved OS was positively associated with lower performance status (HR 0.61, 95% CI 0.41-0.91; p = 0.02), lower T stage (HR 0.59, 95% CI 0.37-0.95; p = 0.03) and receiving primary chemotherapy (HR 0.60, 95% CI 0.40-0.90; p = 0.01). No variables retained significance on multivariable analysis (radiotherapy versus radical cystectomy: HR 0.92, 95% CI 0.61-1.39; p = 0.69).
Dr. Swinton concluded his presentation discussing clinical outcomes in cN+M0 bladder cancer patients with the following take home messages:
- This multi-center retrospective analysis of survival outcomes gives real-world data on a large cohort of patients with cN+M0 bladder cancer
- A limitation of this data is the risk of confounders when comparing retrospective cohorts
- Overall survival unfortunately remains poor in this cohort but was significantly longer in patients who received radical-intent treatment
- There was no difference in overall survival between patients receiving radical cystectomy and radical radiotherapy
- Given the equivalent survival outcomes in these patients whose overall prognosis remains poor, this data would support wider use of radiotherapy to avoid risks from major surgery in node-positive patients
Presented by: Martin Swinton, MD, Christie Hospital, Manchester, United Kingdom
Co-Authors: N. B. G. Mariam2, J. L. Tan3, K. Murphy4, T. Elumalai5, M. Soni6, A. Ferrera7, C. Richardson6, R. Walshaw4, H. Mistry8, V. Ramani1, Y. Song1, A. Birtle9, A. Henry10, J. Chan4, P. Hoskin3, and A. Choudhury11; 1Christie Hospital, Manchester, United Kingdom, 2Manchester University NHS Foundation Trust, Manchester, United Kingdom, 3University of Manchester, Manchester, United Kingdom, 4Clatterbridge Cancer Centre NHS Foundation Trust, Wirral, United Kingdom, 5Addenbrooke's Hospital, Cambridge, United Kingdom, 6St. James's Institute of Oncology, Leeds, United Kingdom, 7Lancashire Teaching Hospitals NHS Foundation Trust, Preston, United Kingdom, 8Division of Pharmacy, University of Manchester, Manchester, United Kingdom, 9Lancashire Teaching Hospitals NHS Foundation Trust, Cancer Oncology, Preston, United Kingdom, 10Leeds Teaching Hospitals NHS Trust, Division of Cancer Studies and Pathology, Leeds, United Kingdom, 11Division of Cancer Sciences, University of Manchester, Manchester, United Kingdom
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Radiation Oncology (ASTRO) Annual Hybrid Meeting, San Antonio, TX, Sat, Oct 22 – Wed, Oct 26, 2022.


