(UroToday.com) The 2022 American Society for Radiation Oncology (ASTRO) Annual Meeting held in San Antonio, TX between October 23rd and 26th, 2022 was host to a State of the Art session for the selection and treatment of localized prostate cancer. Dr. Alexander Lukez presented results of a study evaluating patient reported quality of life after moderately hypofractionated proton beam therapy or intensity modulated radiation therapy for prostate cancer.
Randomized controlled trials have shown that hypofractionated radiation therapy for prostate cancer is feasible, safe, and effective, with such regimens largely using photon-based radiation. Proton beam therapy has potential dosimetric advantages. A recent report comparing proton beam therapy versus photon-based intensity modulated radiation therapy (IMRT) demonstrated low rates of physician-reported GI and GU toxicity. However, it is well-known that physicians may underreport adverse changes in patient quality of life. As such the authors sought to characterize and compare late GI and GU patient-reported outcomes between patients treated with either proton beam therapy or IMRT.
In their study, the authors included patients with biopsy-proven NCCN low- or intermediate-risk prostate cancer treated with definitive radiation to an intact prostate using moderate hypofractionation (defined as 250 – 325 cGy/fraction). Patients receiving photon beam therapy did so with static IMRT or rational arc therapy. Those who received proton-based treatment did so with uniform scanning or pencil beam scanning. Pelvic lymph nodes were not included in the treatment volume. All patients underwent daily 3-dimensional image guidance. Use of ADT was allowed, but not required.
This study was conducted across four tertiary care referral centers with data prospectively collected using patient-reported QoL questionnaires: International Prostate Symptom Score (IPSS) and the Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP) questionnaire, with a particular focus on questions 5 and 6 (GI and GU). Data were collected pre-treatment and subsequently at 3- and 6-month intervals. Statistical analysis was conducted using the Chi-square and student’s t-test. Generalized logistic and linear regression models were conducted evaluating time and type of treatment, as well as their interaction, controlling for other factors including age, race, and NCCN risk group.
This study included 772 patients (287 IMRT and 485 proton beam therapy). Of the four centers included, one center contributed patients to both cohorts. There were some notable differences in the baseline patient characteristics between the two groups:
- Age at diagnosis was higher in the IMRT group (69 versus 66 years, p<0.001)
- There was a greater proportion of intermediate-risk and Gleason Score 7 patients in the IMRT group (81.2% versus 68.2%, p<0.001)
- Rectal balloon was used in 12.4% of proton beam therapy patients (versus none in IMRT)

Starting with IPSS scores, note was made of similar mean baseline IPSS scores between the two groups (p=0.74). On follow up evaluation at 12, 24, and 36 months, there we no significant differences between the proton beam therapy and IMRT cohort, as demonstrated in the box plots below. These results remained consistent after controlling for potential confounders such as age, race, and NCCN risk groups.

Next, evaluating GU moderate or severe toxicity using the EPIC-CP questionnaire, the authors noted overall low rates of significant urinary toxicity. A trend towards worse urinary frequency in the IMRT group at 24 months was noted (OR 0.35, p=0.096).

With regards to GI moderate or severe toxicity, the long-term rates of significant overall bowel symptoms were low. On multivariable regression, there were no significant differences in bowel pain/urgency or bowel frequency symptoms. However, a trend towards worse bowel pain/urgency at 1 year in the proton beam therapy group was noted (1.7% to 4.9%; OR 2.93, p=0/091).

Looking at overall GI toxicity, it appeared that overall GI scores peaked at two years post-treatment. On multivariable analysis, EPIC-CP overall GI toxicity did not significantly differ. Again, at 12 months, there was a trend towards worse 3+ overall GI scores in the proton beam therapy group (OR: 3.68, p=0.085).
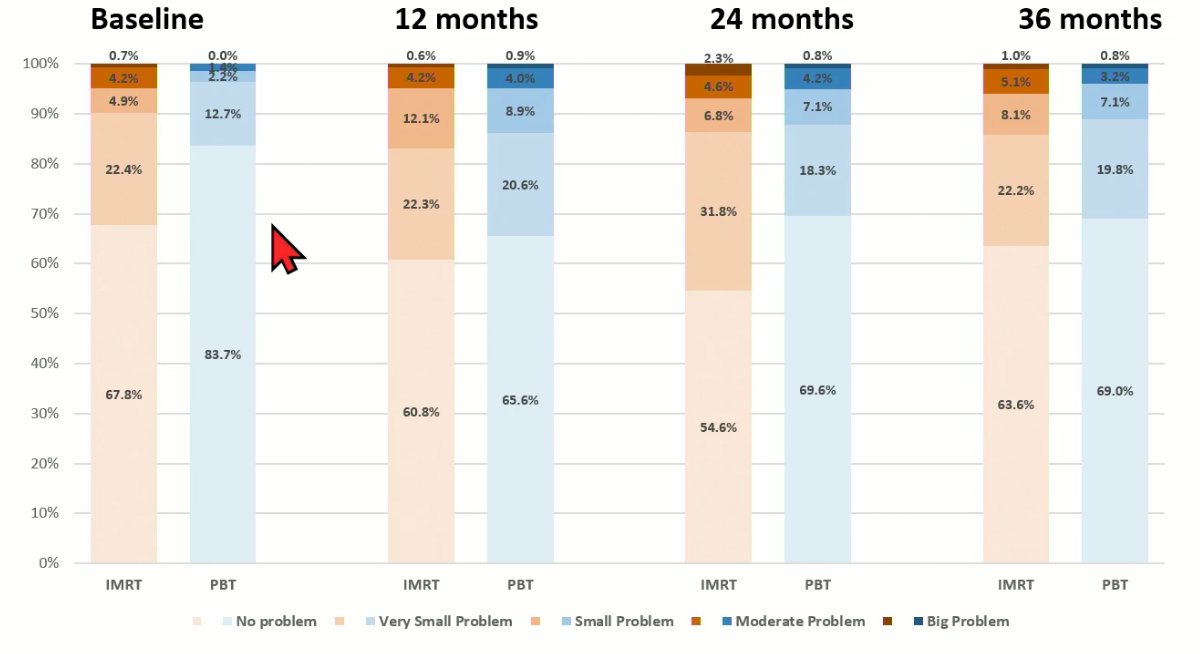
As demonstrated in the figure below, multivariable analysis did not demonstrate any significant differences between the two groups with regards to EPIC GU frequency, GU stream, GI overall, or IPSS scores. Although none reached the threshold of less than 5% type 1 error rate, the EPIC GU frequency scores appeared to be superior in the proton beam therapy arm at 24 months (OR: 0.35, 95% CI: 0.10 – 1.20, p=0.096), whereas the EPIC GI overall scores at 12 (OR: 3.68, p=0.085) and 24 months (OR: 2.78, p=0.26) appeared to favor the IMRT arm.

The authors noted the following limitations to this study:
- This was a collaboration of pooled single institution experiences and not a randomized clinical trial
- There was rreatment heterogeneity with variation in radiation technique between institutions
- Selection bias related to treatment modality decision
- Partial EPIC-CP questionnaire score reporting, which was limited to questions 5 and 6
Dr. Lukez concluded as follows:
- There were no significant differences found in late (years one, two, and three) patient-reported toxicity outcomes between proton beam therapy and IMRT
- Moderately hypofractionated proton beam therapy and IMRT yield low rates of patient-reported late GI and GU toxicity
- We await randomized trials comparing late radiation toxicity outcomes with proton and photon radiation to an intact prostate (i.e. COMPPARE trial, NCT03561220).
Presented by: Alexander Lukez, MD, Resident Physician, Department of Radiation Oncology, Fox Chase Cancer Center, Philadelphia, PA
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2022 American Society of Radiation Oncology (ASTRO) Annual Hybrid Meeting, San Antonio, TX, Sat, Oct 22 – Wed, Oct 26, 2022.


