(UroToday.com) The 2023 ASTRO annual meeting included a session on oligometastatic prostate cancer, featuring a presentation by Dr. Shekinah Elmore discussing cases in oligometastatic prostate cancer and partnering in patient-centered care. Dr. Elmore started by highlighting that her learning objectives were to (i) identify the patient centered and palliative care competencies required in the treatment of patients with oligometastatic prostate cancer, and (ii) to discuss case-based paradigms for the use of radiation for patients with metastatic prostate cancer. She notes that there is not one evidenced-based recommendation that will suit every patient, but she and her team note the “Four P’s” for what is most important for oligometastatic prostate cancer patients:
- Patient goals and values
- Patient reported outcomes and quality of life
- Prognostication
- Palliative and supportive interventions
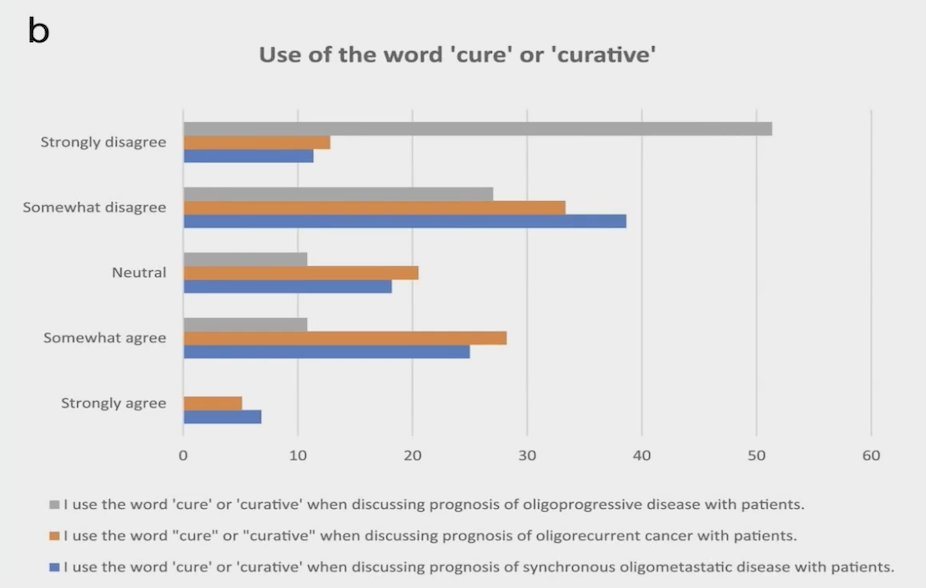
Dr. Elmore highlighted the importance of language and how we speak to our oligometastatic prostate cancer patients. For example, use of the word ‘cure’ or ‘curative’:1
The first case Dr. Elmore discussed was a 71 year old male, ECOG 0, a PSA of 14.4 ng/mL, with Gleason Grade Group 4 prostate cancer in 6/14 cores, 70-80% pattern 4, and no cribriform pattern. His bone scan was subsequently negative and his CT of the abdomen and pelvis showed a 1.6 cm right lower lobe lung nodule. An 18F FDG PET/CT was then performed, which did not demonstrate uptake in the right lower lobe lung nodule, but did show T12 and L4 uptake suspicious for metastatic prostate cancer. Subsequently, an Axumin PET scan confirmed L4 vertebral body uptake and a subtle signal in the right sacrum, but no CT correlation. Dr. Elmore discussed expectations with the patient regarding long-term cancer control (“years”) with long term ADT and a radiation approach. She also discussed alternatives of maximizing time off ADT with a radiation only versus a radiation with short term ADT approach. Finally, she discussed anxiety and fear surrounding a metastatic prostate cancer diagnosis. This patient was eventually treated with moderately hypofractionated radiation to the prostate and pelvis, as well as CyberKnife SBRT to the L2 and L4 vertebral lesions. With regards to systemic therapy, he was treated with 24-36 months of ADT + abiraterone:
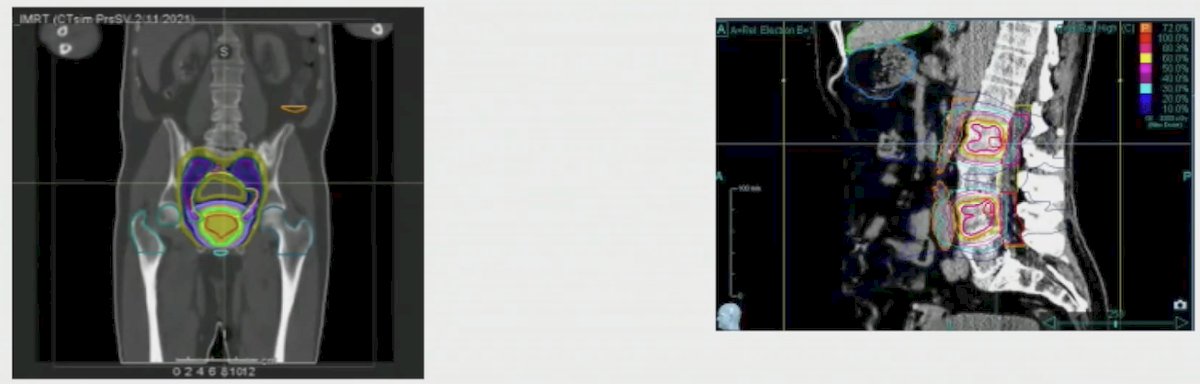
On follow-up, the patient's MRI was stable for six months and his PSA has been undetectable for 28 months.
The second case Dr. Elmore discussed was a 75 year old male, ECOG 0, with a history of SBRT for low risk prostate cancer in 2017. His PSA began to rise to 0.43 ng/mL in June 2022 with the following subsequent trend: 0.70 ng/mL 0.65 ng/mL 0.72 ng/mL. A PSMA PET showed a single left obturator/internal iliac lymph node (1.7 x 1.6 cm) deep to the left gluteal muscle, which interventional radiology was unable to biopsy given the location; there was no uptake in the prostate:

Dr. Elmore discussed several aspects of care with this patient, including (i) patient preference for approach without ADT due to perceived severity of side effects, (ii) potential for microscopic spread in adjacent lymph node chains in addition to visible lymph nodes, (iii) ways to cope with ADT side effects, and (iv) wanting to control this area, hoping that other areas would not appear, and a goal of close surveillance. The patient subsequently underwent LINAC-SBRT to the PET avid disease with 6 months of neoadjuvant, concurrent, and adjuvant ADT:

On his follow-up visit in February 2023, ADT was started, SBRT was completed in April 2023, and his PSA was undetectable in July 2023 (next follow-up October 2023).
Dr. Elmore concluded her presentation by discussing cases of oligometastatic prostate cancer and partnering in patient-centered care with the following take-home points focusing on her institutional heuristics for oligometastatic prostate cancer:
- Newly diagnosed oligometastatic prostate cancer
- Treatment of the prostate with “standard” radiation +/- lymph nodes versus SBRT
- Treatment of all bone metastatic sites with SBRT is safe
- Long-term ADT (18-36 months) +/- the addition of second generation anti-androgens
- Oligorecurrent/oligoprogressive prostate cancer
- Salvage of the primary, if indicated
- Treatment of lymph nodes or bone metastatic disease with SBRT if safe
- At least short-term ADT (6 months), and consider addition of second generation anti-androgens
- All Patients
- Consider the “Four Ps” and individualize accordingly
Presented by: Shekinah Elmore, MD, MPH, UNC Chapel Hill School of Medicine, Chapel Hill, NC
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2023 American Society for Therapeutic Radiation Oncology (ASTRO) 65th Annual Meeting held in San Diego, CA between October 1st and 4th, 2023
References:
- Cho HL, Balboni T, Christ SM, et al. Is Oligometastatic Cancer Curable? A survey of oncologist perspectives, decision making, and communication. Adv Radiat Oncol. 2023 Mar 18;8(5):101221.


