(UroToday.com) The 2023 ASTRO annual meeting included a session on oligometastatic prostate cancer, featuring a presentation by Dr. Phuoc Tran discussing the definition of oligometastatic disease in the PSMA PET era and treatment approach.
Dr. Tran started his presentation by emphasizing that traditional teaching has suggested that localized prostate cancer is curable, whereas metastatic prostate cancer is incurable:
It wasn’t until S. Hellman and R.R. Weichselbaum coined the term “oligometastases” as an intermediate state of cancer spread between localized disease and widespread metastases that we started to shift our thinking and perhaps the “cure line”: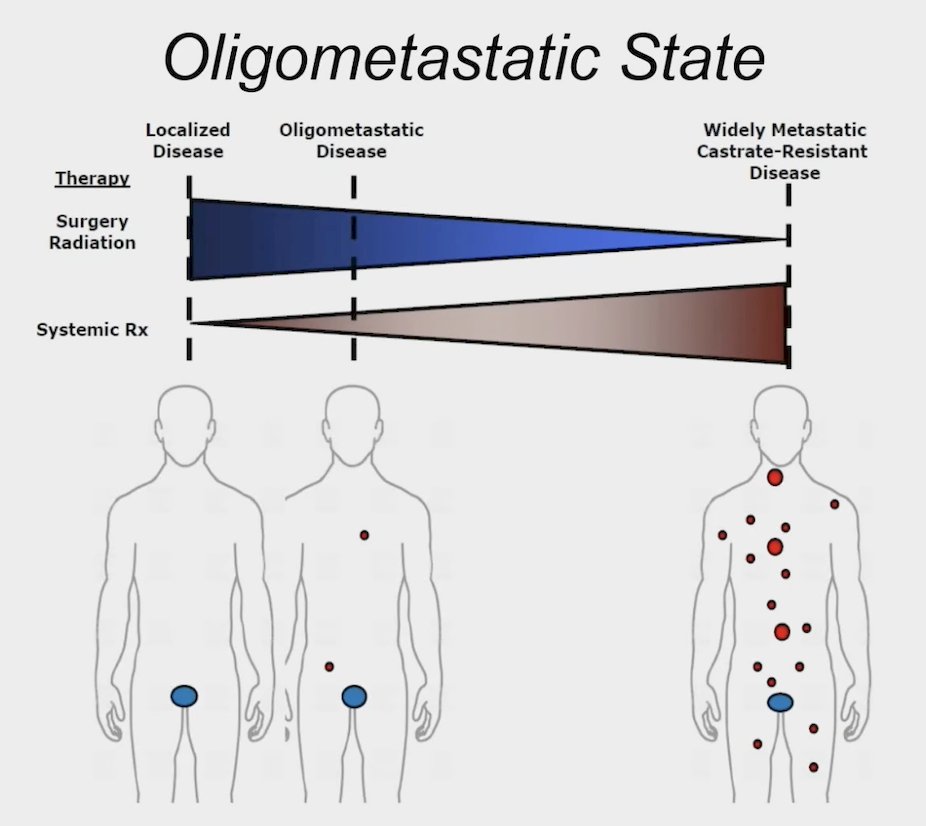
Dr. Tran notes that there is no agreeable “oligometastatic disease burden” definition, but generally, in his practice, he thinks of this as 3-5 metastatic sites. However, with conventional imaging, the metastatic burden we see is often much less than what is present. With the uptake and availability of PSMA PET/CT, perhaps the subclinical disease burden we do not see will be much less. It is important to note that there are several different oligometastatic disease presentations, including de novo or synchronous, oligorecurrent or metachronous, and oligoprogressive: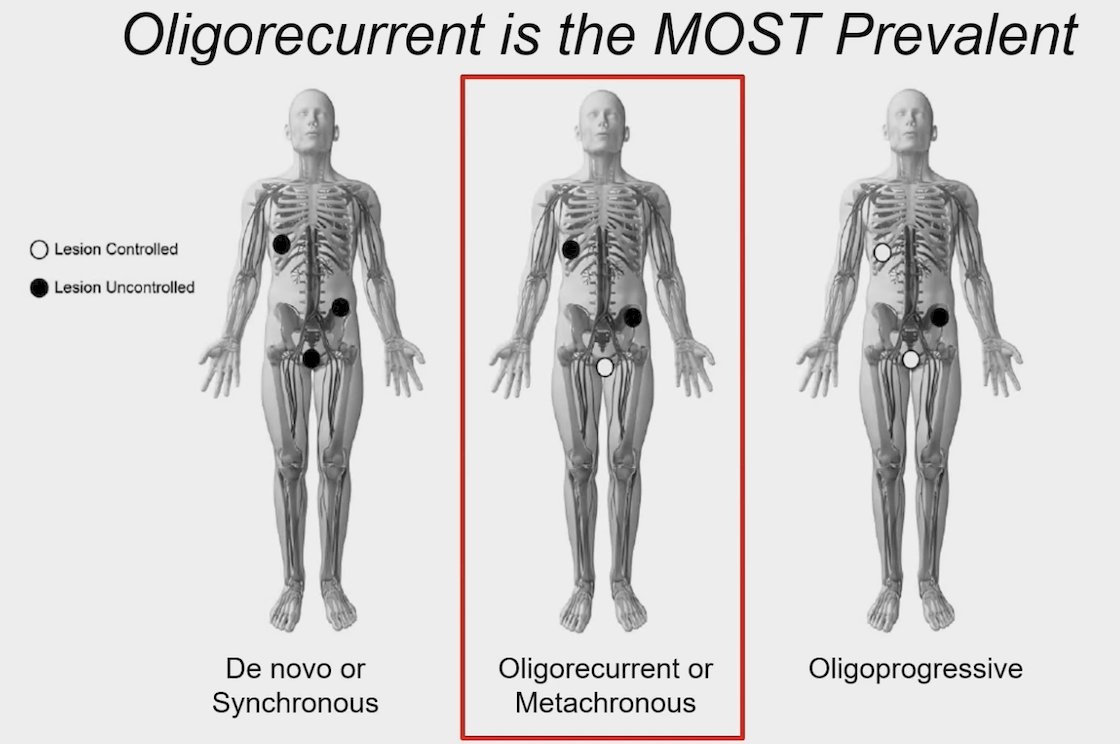
Dr. Tran notes that with a PSA <5 ng/mL, conventional imaging is essentially of no value. However, as we have seen, 18F-PSMA PET and 68Ga-PSMA PET are now the most common imaging modalities, with these molecular imaging options being most sensitive with PSA < 2 ng/mL (in both the de novo and synchronous metastatic setting).
Dr. Tran’s group recently published an analysis assessing the clinical and genomic differences between advanced molecular imaging detected and conventional imaging detected metachronous oligometastatic castration-sensitive prostate cancer.1 Among 295 patients included in this study, patients with conventional imaging detected oligometastatic CSPC had significantly higher Gleason grade group (p = 0.032), higher PSA at oligometastatic CSPC diagnosis (8.0 versus 1.7 ng/ml; p < 0.001), and more frequent pathogenic TP53 mutations (28% versus 17%; p = 0.030):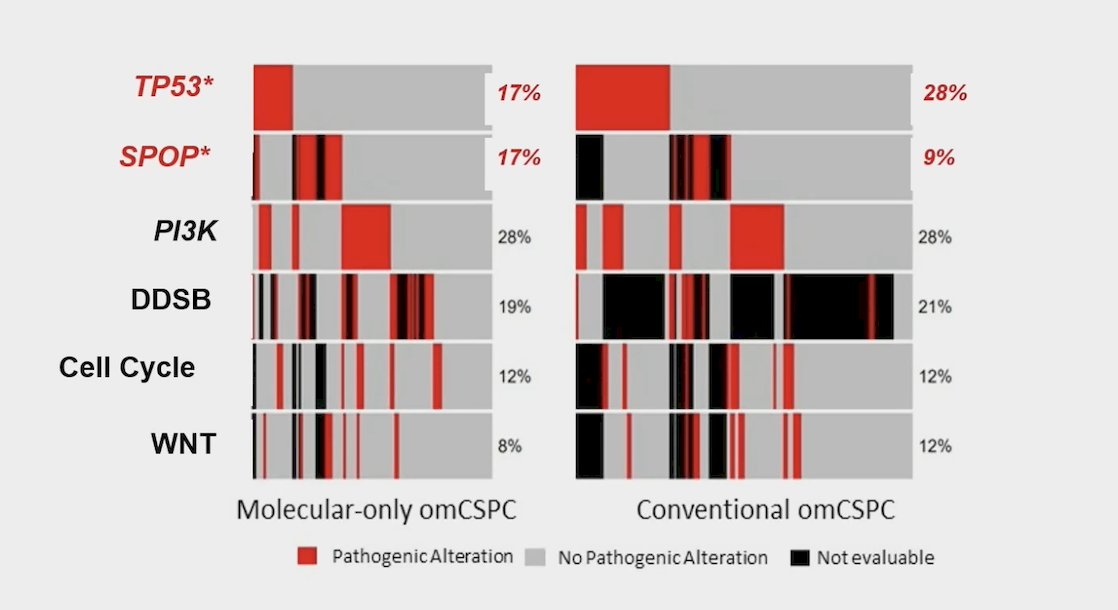
Additionally, patients that had conventional imaging detected oligometastatic CSPC had worse 10 year overall survival (85% versus 100%; p < 0.001): 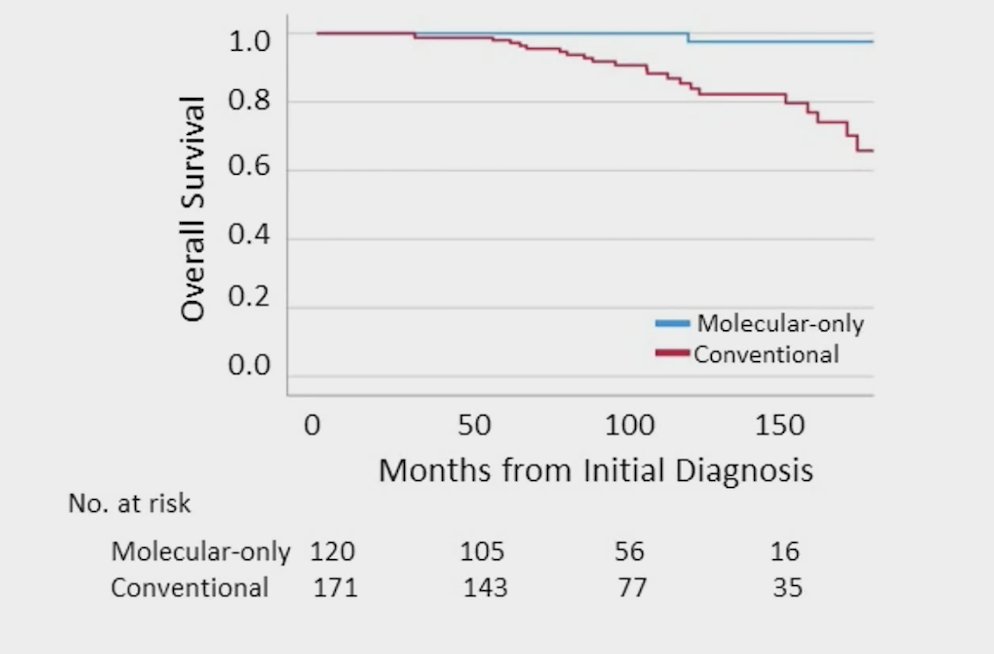
The consolidative hypothesis for how metastases occurs is such that if oligoprogression is a pathway to widely metastatic disease, then consolidative therapies can alter this natural history: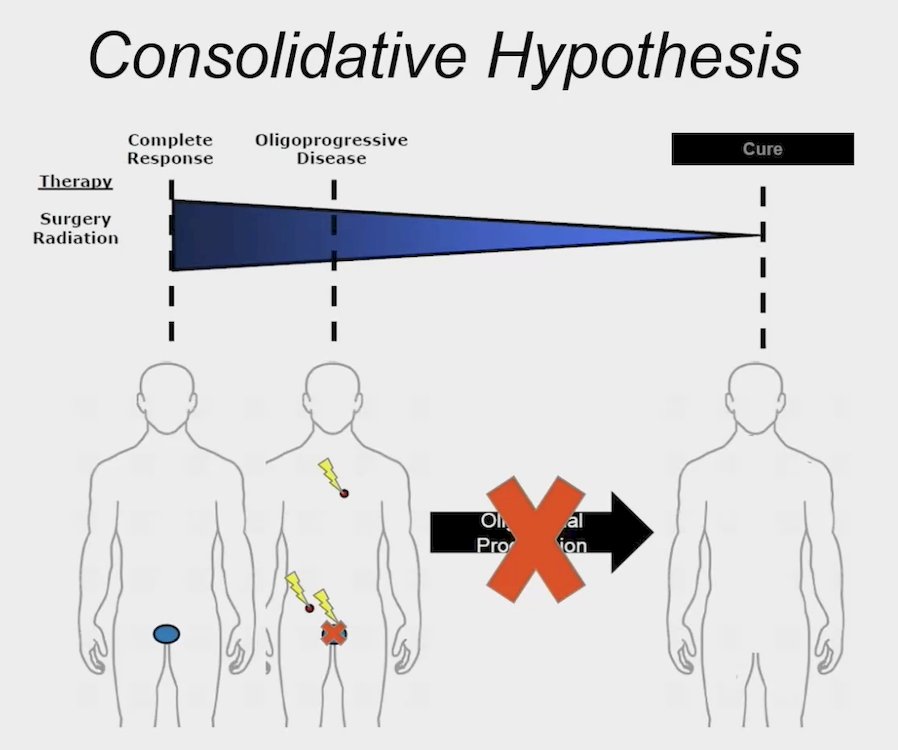
Whether metastasis directed therapy – SABR can alter this natural history of oligoprogression was assessed in the ORIOLE trial.2 Indeed, treatment with stereotactic body radiotherapy improved median progression-free survival (not reached vs 5.8 months; HR 0.30, 95% CI 0.11-0.81; p = 0.002):
What also was assessed in the ORIOLE trial is whether consolidative PSMA-guided metastasis directed therapy – SABR can alter the natural history of the disease. In ORIOLE, there were 19 patients with total consolidation of their oligometastases, whereas 16 patients had subtotal consolidation:
Assessing distant metastasis free survival, those patients that had total consolidation versus those with subtotal consolidation had significantly improved outcomes (HR 0.19, 95% CI 0.07-0.54):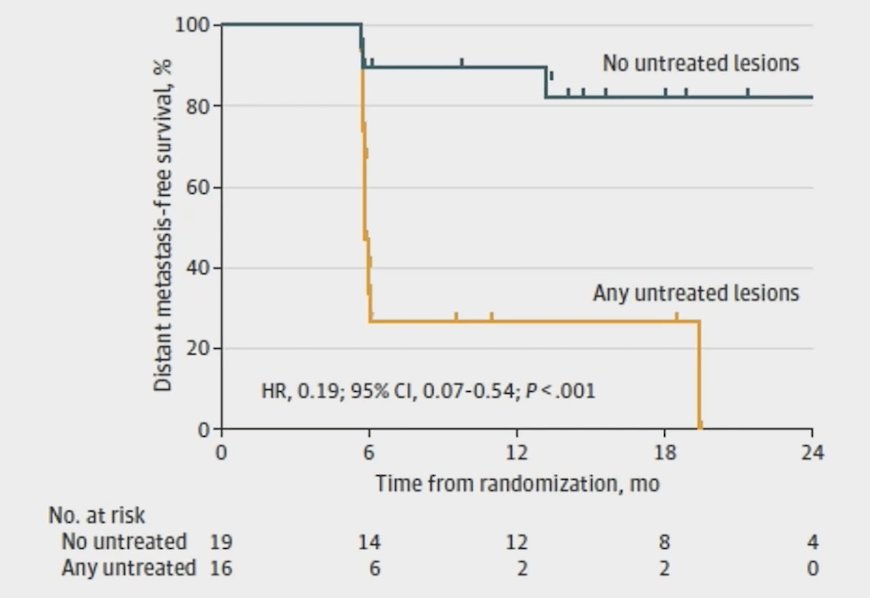
To discuss how metastasis directed therapy – SABR modulates PSMA PET/CT, Dr. Tran presented some unpublished data from his group. Assessing change from pre-metastasis directed therapy PSMA SUV, treated lesions had a substantial decrease in SUV versus those lesions that were untreated: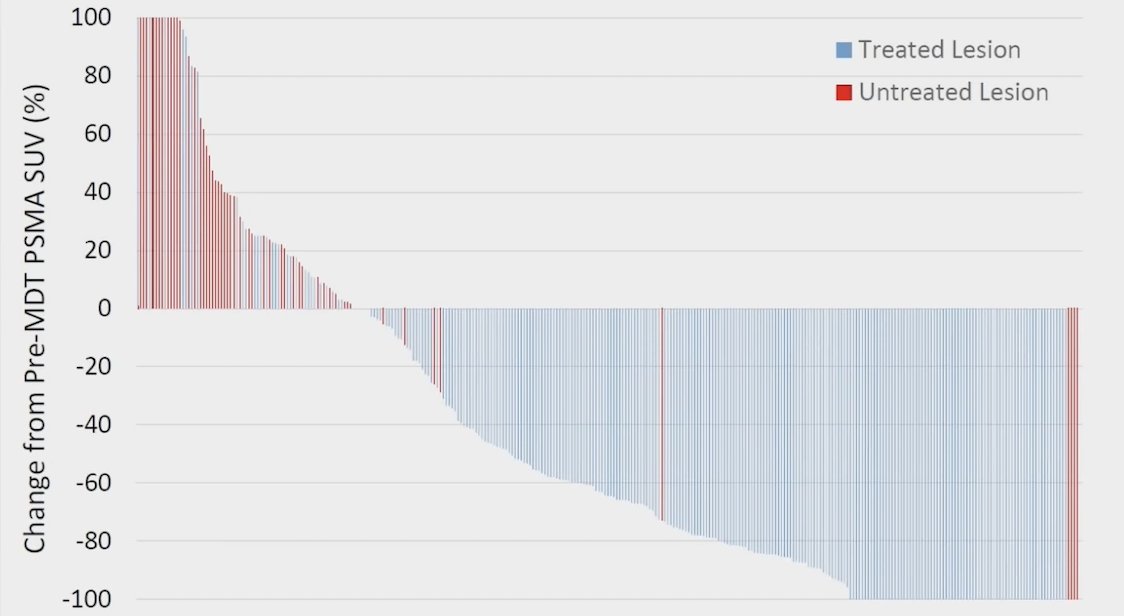
Importantly, these PSMA lesion responses also correlated with outcomes, with significantly improved metastasis free survival: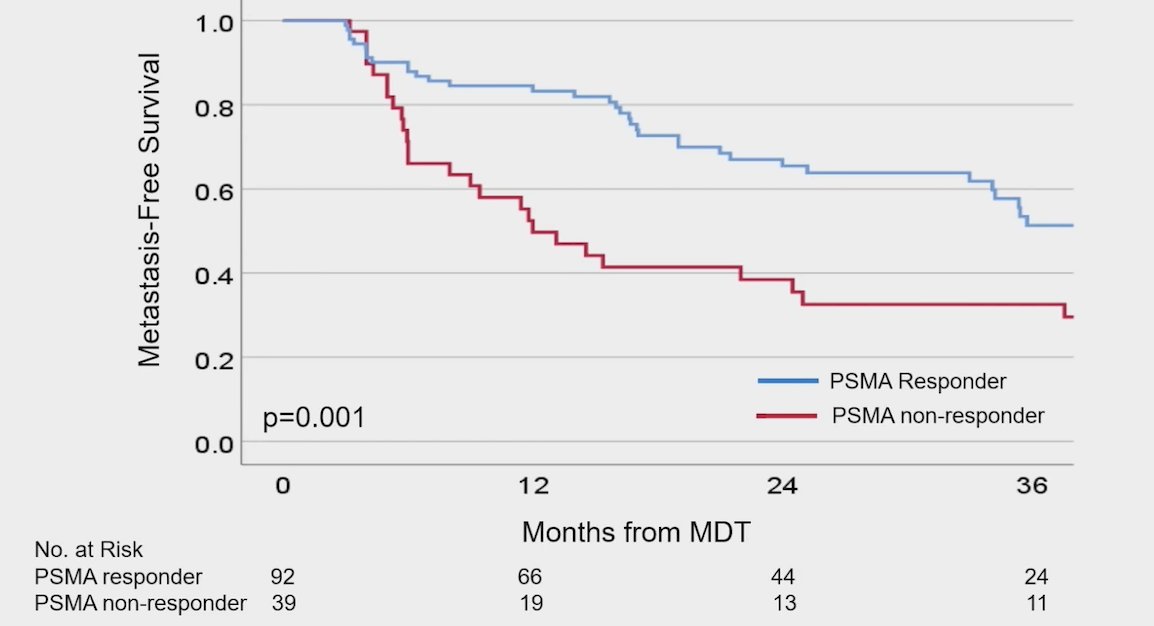
Dr. Tran concluded this presentation discussing the definition of oligometastatic disease in the PSMA PET era and treatment approach with the following take-home points:
- PSMA PET positive oligometastatic CSPC patients may constitute a distinct subtype of clinical-biological disease
- ORIOLE demonstrated that metastasis directed therapy-SABR is safe in recurrent oligometastatic castration sensitive prostate cancer
- ORIOLE also suggested that consolidative local treatment can alter the natural history of oligometastatic CSPC and that PSMA PET-guided metastasis directed therapy consolidation may alter metastatic disease progression. The SABR-COMET, STOMP, and EXTEND trials have also shown an improvement in overall survival, ADT-free survival, and eugonadal progression free survival, respectively
- Additional PSMA-targeted imaging research is needed in oligometastatic CSPC. PSMA PET-CT avidity in general decreases following metastasis directed therapy-SABR and may be a response indicator for metastasis free survival. This may be an opportunity to interface with genomics and biomarkers
Presented by: Phuoc Tran, MD, University of Maryland, Baltimore, MD
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2023 American Society of Radiation Oncology (ASTRO) Annual Meeting, San Diego, CA, Sun, Oct 1 – Wed, Oct 4, 2023.
References:
- Sutera P, Song Y, Van der Eecken K, et al. Clinical and Genomic Differences Between Advanced Molecular Imaging-detected and Conventional Imaging-detected Metachronous Oligometastatic castration-sensitive prostate cancer. Eur Urol. 2023 May 10;S0302-2838(23)02790-2.
- Phillips R, Shi WY, Deek M, et al. Outcomes of Observation vs Stereotactic Ablative Radiation for Oligometastatic Prostate Cancer: The ORIOLE Phase 2 Randomized Clinical Trial. JAMA Oncol 2020 Mar 26;6(5):650-659.


