(UroToday.com) The 2023 American Society for Radiation Oncology (ASTRO) 65th Annual Meeting held in San Diego, CA between October 1st and 4th, 2023 was host to a session discussing combined modality therapy for lymph node positive prostate cancer. Dr. Rahul Tendulkar led the session with a case presentation of a 51-year-old male found to have an elevated PSA of 16 ng/ml. He subsequently underwent an MRI which demonstrated a PIRADS 5 lesion with evidence of extraprostatic extension.
Subsequent biopsy demonstrated Grade Group 5 disease in 7/12 cores. A staging PSMA-PET/CT demonstrated avidity in the left prostate gland and uptake in a single right external iliac lymph node. Following a tumor board discussion, the treating urologist recommended a radical prostatectomy plus a pelvic lymph node dissection. 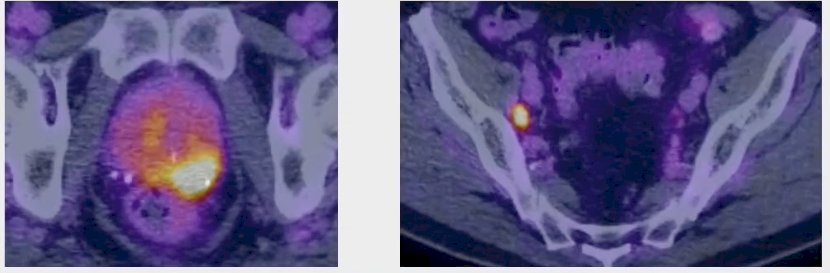
Several important questions arise in this situation:
- Is unimodal therapy sufficient or is there a role for bimodal or trimodal therapy?
- Who needs treatment intensification versus de-intensification – both from local and systemic aspects?
- What is the impact of advanced imaging on staging and management?
- What are some special considerations for cN1 versus pN1 disease?
Following this introduction, Dr. Leslie Ballas proceeded to discuss post-operative therapy for patients with pathologic node positive prostate cancer. Dr. Ballas began by noting that the pN+ population remains understudied. Up to 13% of prostate cancer patients have regional disease at diagnosis. Currently, the only randomized data for pN+ patients comes from the ECOG 3886 trial, which established adjuvant ADT as standard of care.1 For patients with detectable or rising PSA following prostatectomy, early salvage radiotherapy is currently the standard treatment. However, pN+ patients are significantly under-represented in the trials of early salvage versus adjuvant radiotherapy:
- Only 2 patients with pN+ disease in S8794, EORTC 22911, and ARO 96-02
- Only 66 patients (5%) in RADICALS-RT
- Only 27% in GETUG
- RAVES – 0 reported
Which pN+ positive patients may benefit from adjuvant therapy? This decision may be informed by data from 2 retrospective series. In 2004, Daneshmand et al. published the results of a series of 1,936 radical prostatectomy patients, of whom 12% had pN+ disease. The 10-year recurrence-free survival was significantly worse in patients with increased number of involved nodes (5+: 49% versus 1-2: 70%).2 Furthermore, patients with LN density >20% had an increased risk of recurrence. In 2014, Touijer et al. published an analysis of the MSKCC series of 369 pN+ patients and demonstrated that higher Gleason score (>7) and 3+ positive lymph nodes were associated with worse biochemical recurrence outcomes.3
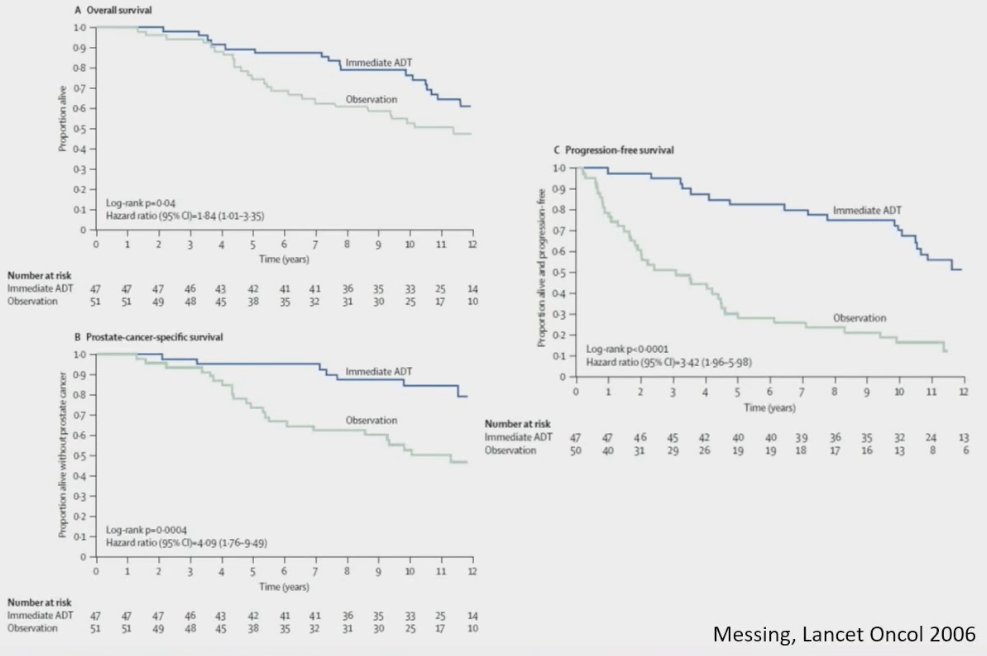
The only randomized trial evaluating the role of immediate versus delayed ADT for pN+ patients was the ECOG 3886 trial, published by Messing et al. in 2006. This trial randomized 98 patients to immediate versus delayed (at time of distant metastases or symptomatic recurrences) lifelong ADT in pN+ patients. The median number of involved nodes was 2. Immediate ADT was associated with significant improvements in:
- Overall survival: HR=1.84
- Cancer specific survival: HR= 4.09
- Progression-free survival: HR= 3.42
But is the ‘problem solved’ with the addition of ADT. Subsequent retrospective data published over the following decade has demonstrated that the 10-year CSS is ~85% in this setting. However, several predictors of adverse survival outcomes remained and included an increased number of involved nodes and higher Gleason score (8 – 10).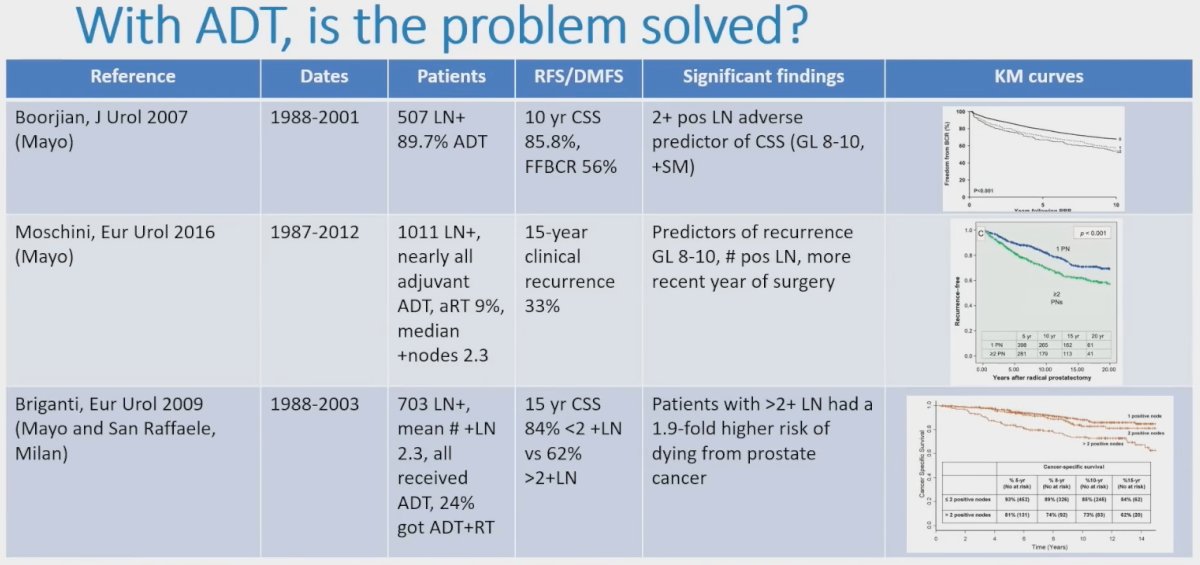
What about adding radiotherapy to surgery and ADT in this setting? A study by Abdollah et al. published in The Journal of Clinical Oncology in 2014 included 1,107 patients, all of whom received ADT and 35% got additional radiotherapy. Adjuvant radiotherapy improved cancer-specific mortality (HR= 0.37, p<0.001). Notably, patients with a pathologic nodal count of 2 or less, Gleason score 7-10, pT3b-4 disease, or positive surgical margins benefited the most. A subsequent analysis by Briganti et al. in 2011 also demonstrated that use of radiotherapy with ADT was associated with improved cancer-specific and overall survivals (by 2.5 fold) at 5, 8, 10 years following surgery, with higher survival rates among patients with 2 or less positive nodes.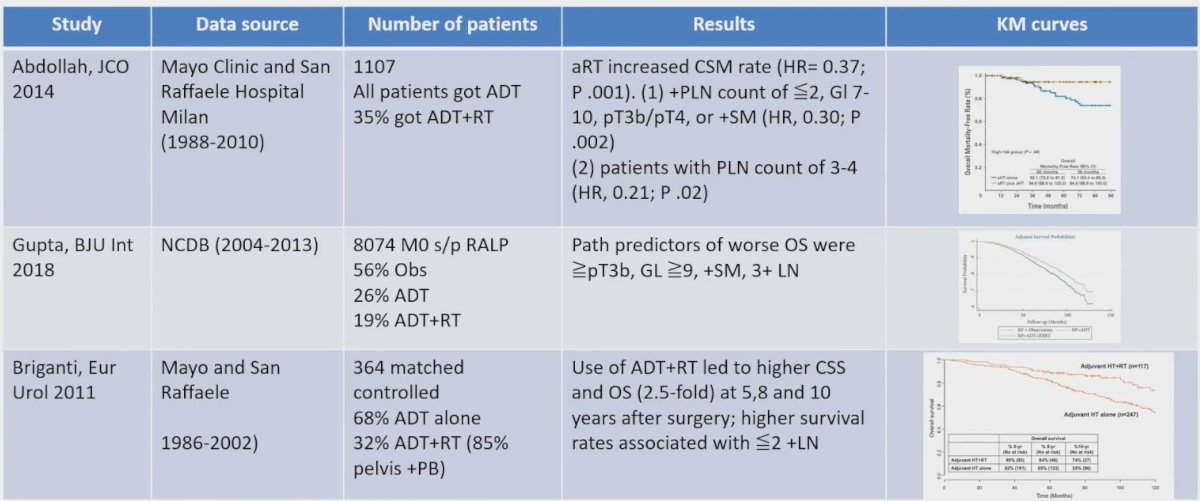
More recently, Touijer et al. in 2018 published an analysis of 1,338 patients with pN+ disease between 1988 and 2010 from 3 institutions (MSKCC, Mayo Clinic, San Raffaele), of whom 28% were observed until PSA failure, 49% received ADT alone, and 23% received ADT + radiotherapy (whole pelvic radiotherapy at 68 Gy). Significantly, treatment with ADT + radiotherapy was associated with better overall survival than ADT alone or observation (HR: 0.41, p<0.001).4 Furthermore, the authors developed a points-based risk stratification system to predict the risk of 10-year all-cause mortality by adjuvant treatment group based on known risk factors of pathologic Gleason score, stage, margin status, and number of positive nodes, with an increased magnitude of benefit for adjuvant therapy with an increased risk score.
Based on this data, there appears to be a benefit to the addition of adjuvant/salvage radiotherapy to ADT for patients with pN+ disease. What about the timing of radiotherapy (adjuvant versus early salvage)? Two studies published by Tilki et al. have demonstrated that adjuvant radiotherapy may be the preferred option in this setting. The first study included 2,424 men with adverse pathology (i.e., pT3-4, Gleason score 8-10), including pN1. This study demonstrated that patients receiving adjuvant radiotherapy had superior all-cause mortality, as demonstrated below:
A subsequent analysis of this cohort demonstrated that the benefit of adjuvant radiotherapy, compared to salvage or no radiotherapy, was most pronounced in those with 4+ positive lymph nodes. There was an 8% reduction in the risk of all-cause mortality for each additional positive lymph node. However, we note that these findings are from an era preceding the widespread use of PSMA PET.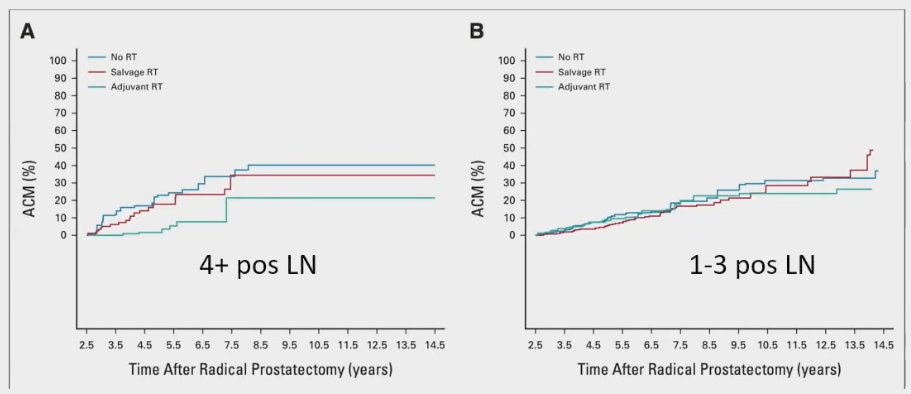
In addition to the number of pathologic nodes involved, does the pre-radiotherapy PSA level play a role in predicting subsequent failure outcomes? An abstract presented at ASTRO 2023 demonstrated that among patients with pN1 disease receiving radiotherapy + ADT, those with a higher pre-radiotherapy PSA had significantly worse biochemical recurrence-free survival rates:
Finally, Dr. Ballas concluded her presentation by noting that the NRG-GU008 trial will assess the role of apalutamide in patients with pN+ disease following a radical prostatectomy receiving radiotherapy + ADT. The trial schema is summarized below.
Presented by:
- Rahul Tendulkar, MD, FASTRO, Associate Professor, Department of Radiation Oncology, Cleveland Clinic, Cleveland, OH
- Leslie Ballas, MD, Department of Radiation Oncology, Cedars-Sinai Medical Center, Los Angeles, CA
Written By: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Society for Therapeutic Radiation Oncology (ASTRO) 65th Annual Meeting held in San Diego, CA between October 1st and 4th, 2023
References:- Messing EM, Manola J, Yao J, et al. Immediate versus deferred androgen deprivation treatment in patients with node-positive prostate cancer after radical prostatectomy and pelvic lymphadenectomy. Lancet Oncol. 2006;7(6):472-9.
- Daneshmand S, Quek ML, Stein JP, et al. Prognosis of patients with lymph node positive prostate cancer following radical prostatectomy: long-term results. J Urol. 2004;172(6 Pt 1):2252-5.
- Touijer KA, Mazzola CR, Sjoberg DD, et al. Long-term outcomes of patients with lymph node metastasis treated with radical prostatectomy without adjuvant androgen-deprivation therapy. Eur Urol. 2014;65(1):20-5.
- Touijer KA, Karnes RJ, Passoni N, et al. Survival Outcomes of Men with Lymph Node-positive Prostate Cancer After Radical Prostatectomy: A Comparative Analysis of Different Postoperative Management Strategies. Eur Urol. 2018;73(6):890-6.


