(UroToday.com) The 2024 ASTRO annual meeting included a session on the management of small cell neuroendocrine tumors of the genitourinary tract, featuring a presentation by Dr. Vedang Murthy discussing radiation therapy for small cell bladder cancers. Dr. Murthy started with a clinical case of a 53-year-old female who underwent a TURBT that showed 95% small cell carcinoma histology and 5% urothelial. The staging CT scan is as follows, confirming T3N1M0 small cell carcinoma of the bladder: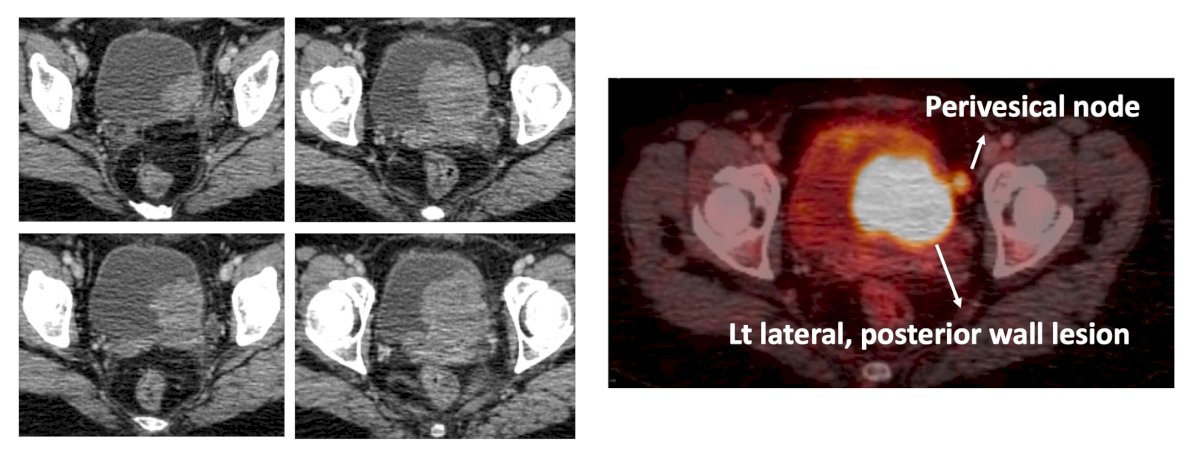
The first question with regards to treatment decisions is whether neoadjuvant chemotherapy is appropriate for this patient. A historical series at MD Anderson Cancer Center from 2004 notes that among 46 patients, neoadjuvant chemotherapy followed by surgery improved survival compared to surgery alone. A follow-up of this series in 2013 showed that among 172 patients, neoadjuvant chemotherapy followed by surgery improved survival compared to adjuvant chemotherapy or no chemotherapy.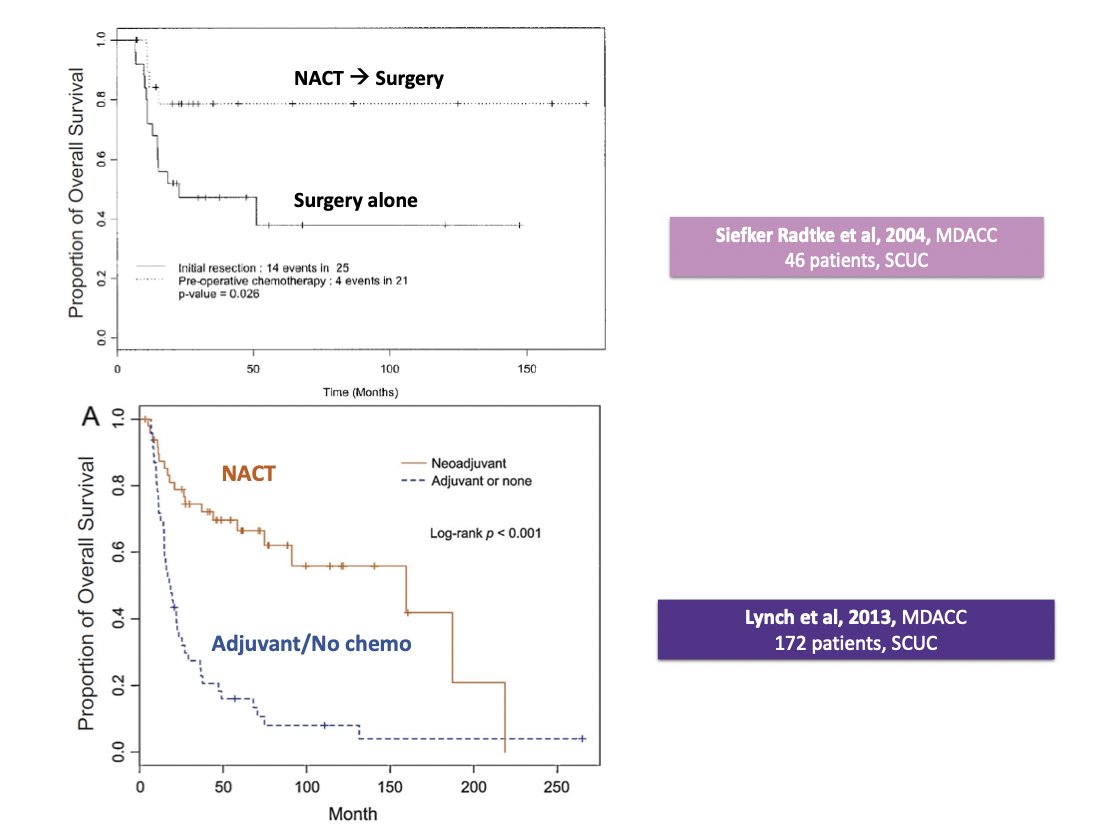
Dr. Murthy notes that the clinical guidelines agree that neoadjuvant chemotherapy is preferred over adjuvant chemotherapy:
- EAU: “Bladder urothelial carcinoma with small cell neuroendocrine variant should be treated with neoadjuvant chemotherapy followed by consolidating local therapy”
- AUA/ASCO/ASTRO/SUO: “For histologic subtypes, neoadjuvant chemotherapy is preferred over adjuvant chemotherapy”
The patient in the aforementioned case did undergo neoadjuvant chemotherapy with 3 cycles of cisplatin + etoposide, with a complete response to the primary lesion: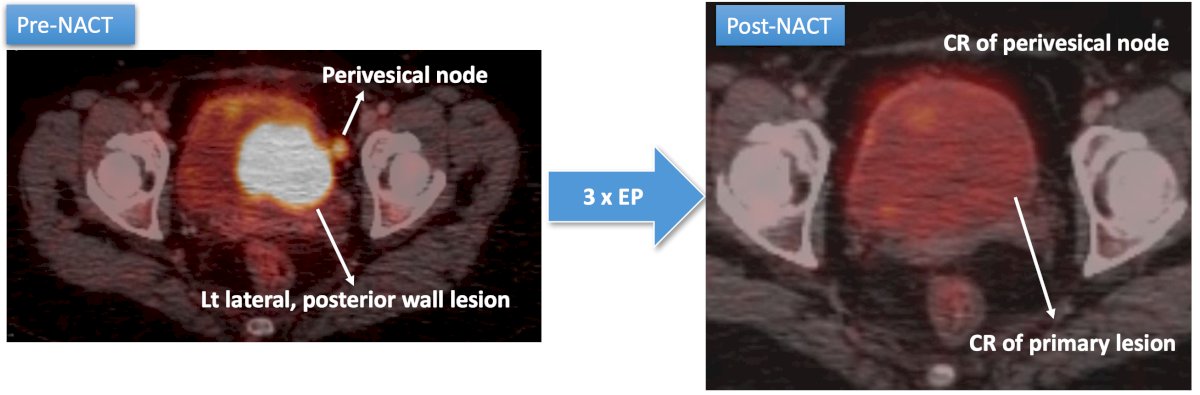
The second question in a treatment decision is whether or not local therapy is needed. Both an NCDB and Memorial Sloan Kettering Cancer Center showed that chemotherapy + local therapy is better than chemotherapy alone: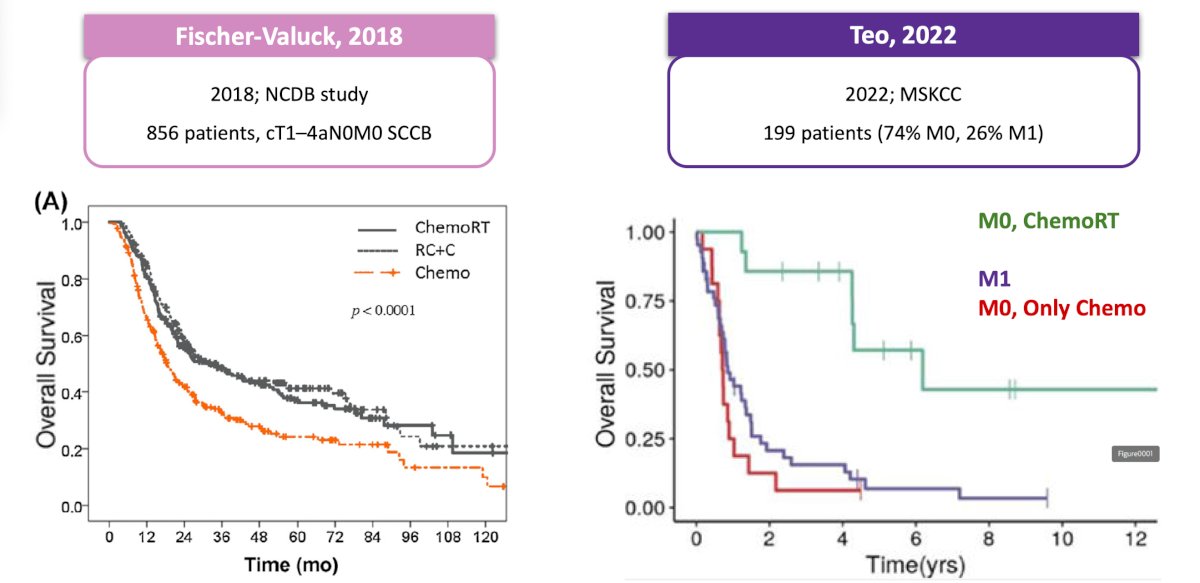
The third question in a treatment decision is what type of local treatment should we choose? Surgery or radiotherapy? Based on limited retrospective evidence, a study from the UK (n = 61 for radical cystectomy vs n = 104 for radiotherapy) and a study from Canada (n = 33 for trimodality therapy vs n = 44 for radical cystectomy) showed that essentially radiotherapy and radical cystectomy are likely equivalent with regards to local therapy in neuroendocrine bladder cancer: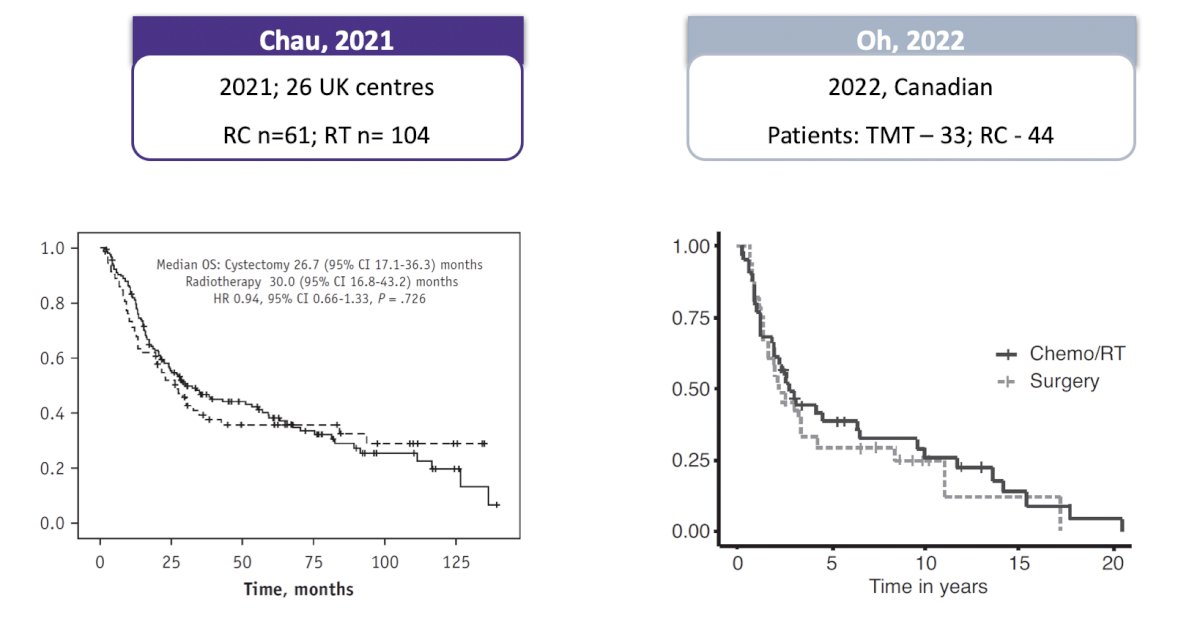
Additionally, an NCDB study from 2020 [1] looked at outcomes among patients with variant muscle-invasive bladder cancer to better assess the role of bladder-preserving chemoradiotherapy versus radical cystectomy.1 Among 356 patients that had bladder-preserving chemoradiotherapy and 2,093 patients that had radical cystectomy, using propensity score weighted analysis, there was no statistical significant difference in overall survival for patients with bladder-preserving chemoradiotherapy as compared to cystectomy (p = 0.387). Additionally, for neuroendocrine, micropapillary, or not otherwise specified histology subgroups, there was no significant difference: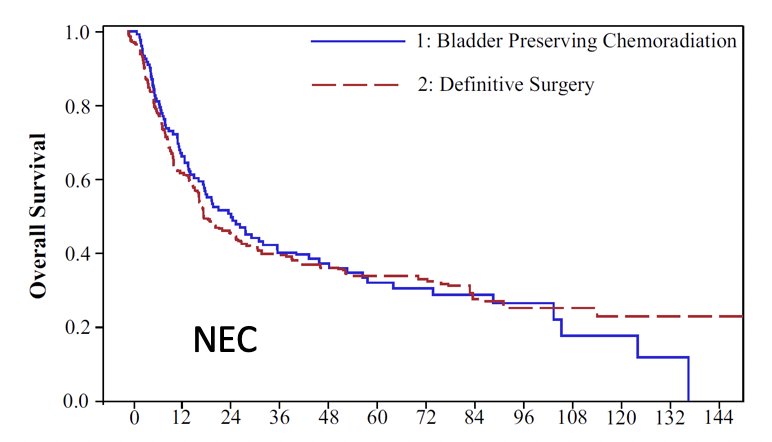
However, patients with adenocarcinoma (HR 1.75) or squamous cell carcinoma (HR 1.49) had worse overall survival associated with bladder-preserving chemoradiotherapy compared to radical cystectomy.
For those that choose radiotherapy, the next question with regards to a treatment decision is what is the volume, dose, fractionation schedule for treatment, and whether prophylactic cranial irradiation should be used? For radiotherapy volume, specifically whole bladder versus partial (tumor/bed), Dr. Murthy notes that there is no definitive data, but studies assessing radical versus partial cystectomy for these patients suggest no difference in cancer-specific survival for bladder neuroendocrine carcinoma, thus both options seem reasonable. Should we treat the pelvis electively? The rationale is that this is an avenue for systemic metastasis, and IMRT with IG-ART allows safe treatment. In a recent study by Halstuch et al. [2] assessing survival outcomes of pure urothelial to histologic subtypes of urothelial carcinoma after radiotherapy, they found the following for radiotherapy to the bladder only versus whole pelvis with regards to metastasis-free survival, cancer-specific survival, and overall survival.
Can we provide these patients with hypofractionated radiotherapy? Dr. Murthy notes that in an individual patient data meta-analysis of the BC2001 and BCON trials,3 over a median follow-up of 120 months (IQR 99-159), patients who received 55 Gy in 20 fractions had a lower risk of invasive locoregional recurrence than those who received 64 Gy in 32 fractions (adjusted HR 0.71, 95% CI 0.52-0.96). Additionally, both schedules had similar toxicity profiles (adjusted RD -3.37%, 95% CI -11.85 to 5.10):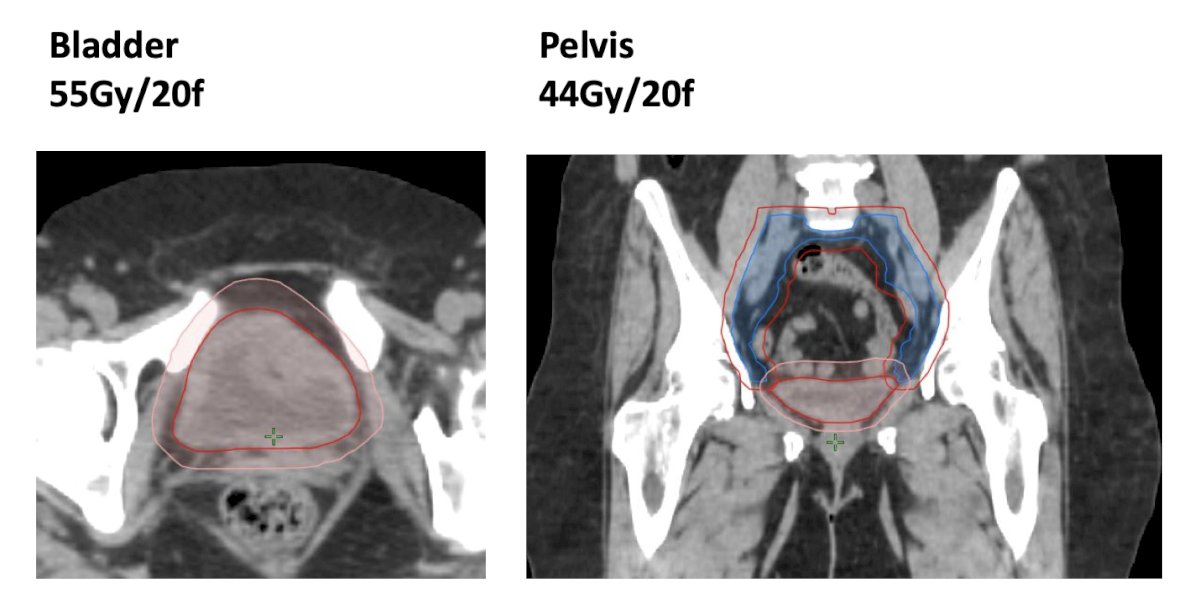
Finally, should we consider prophylactic cranial irradiation? Dr. Murthy notes that for a patient with >= T3bN+M1 neuroendocrine carcinoma of the bladder, there is a brain metastasis risk of ~50%. Presented at ASCO GU 2022, Choi and colleagues noted that among 24 patients with bulky, high stage small cell urothelial cancer, the risk of brain metastases decreased from ~50% to 14% after prophylactic cranial irradiation (24 Gy/10 fractions).
Dr. Murthy concluded his presentation discussing radiation therapy for small cell bladder cancers with the following key takeaways for providing treatment options for these patients: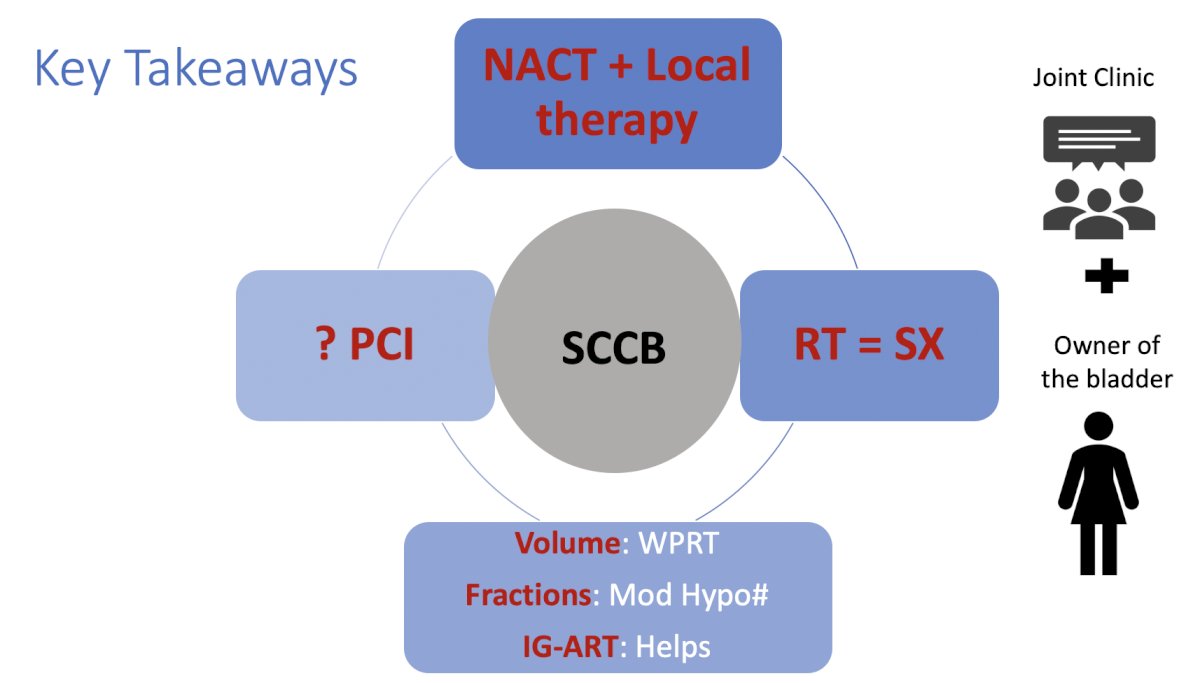
Presented by: Vedang Murthy, MD, DNB, DipEPP, Professor and Radiation Oncologist, Tata Memorial Centre, New Mumbai, Maharashtra, India
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Society for Radiation Oncology (ASTRO) Annual Meeting, Washington, DC, Sun, Sept 29 – Wed, Oct 2, 2024.
References:
- Janopaul-Naylor JR, Zhong J, Liu Y, et al. Bladder preserving chemoradiotherapy compared to surgery for variants of urothelial carcinoma and other tumor types involving the bladder: An analysis of the National Cancer Database. Clin Transl Radiat Oncol. 2020 Nov 9;26:30-34.
- Halstuch D, Kool R, Marcq G, et al. The Impact of Histologic Subtypes on Clinical Outcomes After Radiation-Based Therapy for Muscle-Invasive Bladder Cancer. J Urol. 2024 Jul 25 [Epub ahead of print].
- Choudhury A, Porta N, Hall E, et al. Hypofractionated radiotherapy in locally advanced bladder cancer: An individual patient data meta-analysis of the BC2001 and BCON trials. Lancet Oncol. 2021 Feb;22(2):246-255.


