(UroToday.com) The 2024 American Society for Radiation Oncology (ASTRO) Annual Meeting held in Washington, DC between September 29th and October 2nd, 2024, was host to a prostate cancer treatment intensification session. Dr. Noelia Sanmamed presented the quality-of-life outcomes results from a randomized clinical trial of hypofractionated radiotherapy for intermediate-risk prostate cancer.
Dr. Sanmamed noted that radiotherapy is a treatment option in the curative management of prostate cancer, with long-term disease control rates similar to those observed with radical prostatectomy.1 Three large randomized controlled trials have demonstrated that moderate hypofractionation is non-inferior to conventional fractionation for the treatment of prostate cancer patients.2-4
The PROFIT trial compared conventional fractionation (78 Gy in 39 fractions) to moderate hypofractionation (60 Gy in 20 fractions) and demonstrated an 85% disease-free survival rate at 5 years, with no significant differences in gastrointestinal or genitourinary toxicities.2 These results have led to recommending moderate hypofractionation as a standard of care option for the treatment of prostate cancer patients.
The study objective was to compare patient-reported outcomes following treatment with moderate hypofractionation (60 Gy in 20 fractions over 4 weeks) to conventional fractionation (78 Gy in 39 fractions over 8 weeks).
This trial included a total of 1,206 intermediate-risk patients who were randomized to either conventional fractionation (n=598) or moderate hypofractionation (n=608).
Patient-reported outcomes were evaluated at baseline, 24 months, and 48 months. The minimally important difference (MID) was defined as a deterioration in health-related quality of life scores at each time point, compared to baseline, by ≥0.5 standard deviations.
The Pearson’s Chi-square test was used to compare the MID between the two arms at each visit. To compare each domain score between arms, multivariable linear regression analysis was performed. Statistical significance was set at p<0.01. Statistical analyses were performed using R version 4.3.0.
The questionnaire completion rates are summarized below. At baseline, almost 90% of patients completed the questionnaire. This dropped to ~80% at 24 months and was slightly lower at 48 months.
Overall, there were no differences in urinary symptoms scores between conventionally and moderately hypofractionated-treated patients.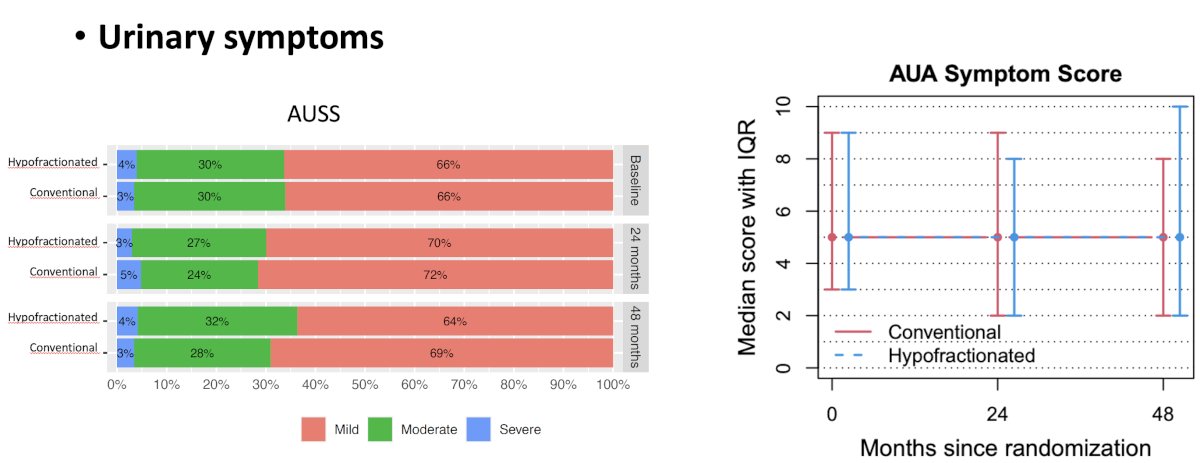
There were no statistically significant or clinically meaningful differences in any of the following EPIC domains (urinary, sexual, hormonal) between the two treatment arms. On average, there was a similar 10-point decrease in the mean sexual domains score. However, the bowel summary scores were superior in the conventional fractionation-treated patients at 48 months (p=0.01).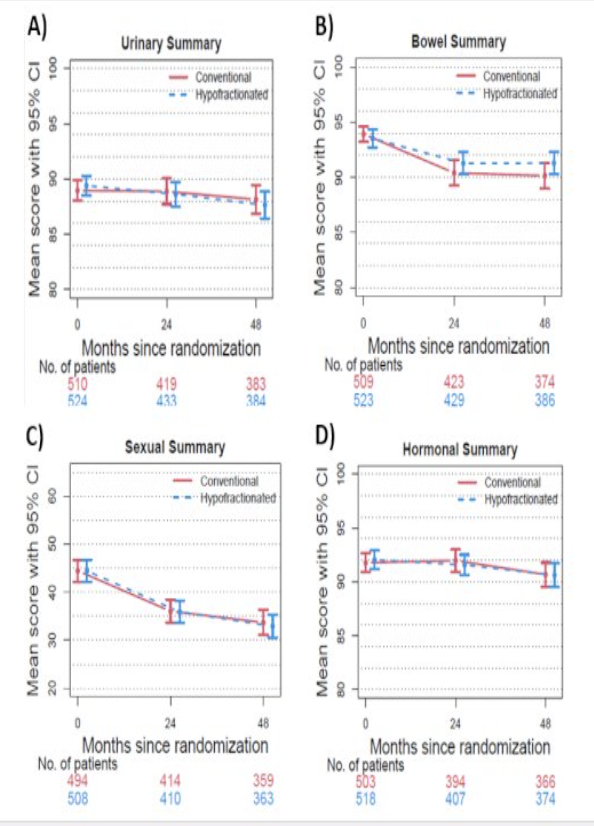
The urinary function and incontinence subdomains scores showed a decline of ~5 points. The urinary bother and irritative subdomain scores remained stable.
With regards to the EPIC bowel subdomains, both the bowel function and bother subdomain scores decreased over time. The biggest decrease was in bowel both – five points in the conventional fractionation arm and three points in the hypofractionated arm. These reached a nadir by 24 months and remained stable through to month 48.
For the EPIC sexual subdomains, both sexual function and bother decreased by ≥10 points from baseline to month 24 in both arms.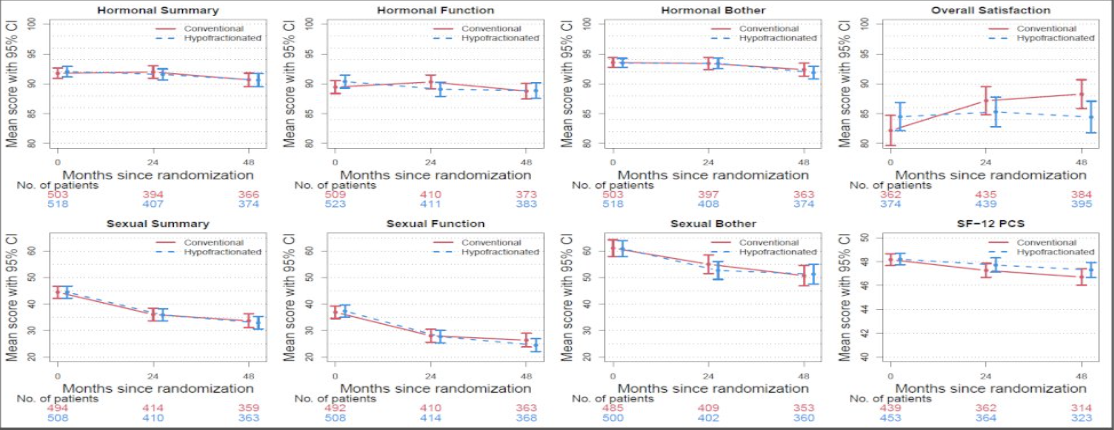
The hormone subdomains remained stable, although the study investigators found a significant difference in hormonal function in favor of the conventional fractionation arm at 24 months that was not maintained at 48 months. Dr. Sanmamed noted that this finding may be a spurious one as ADT was not allowed during the treatment phase of the study, and very few patients had initiated salvage LHRH agonist therapy by 24 months (only one patient in each study arm).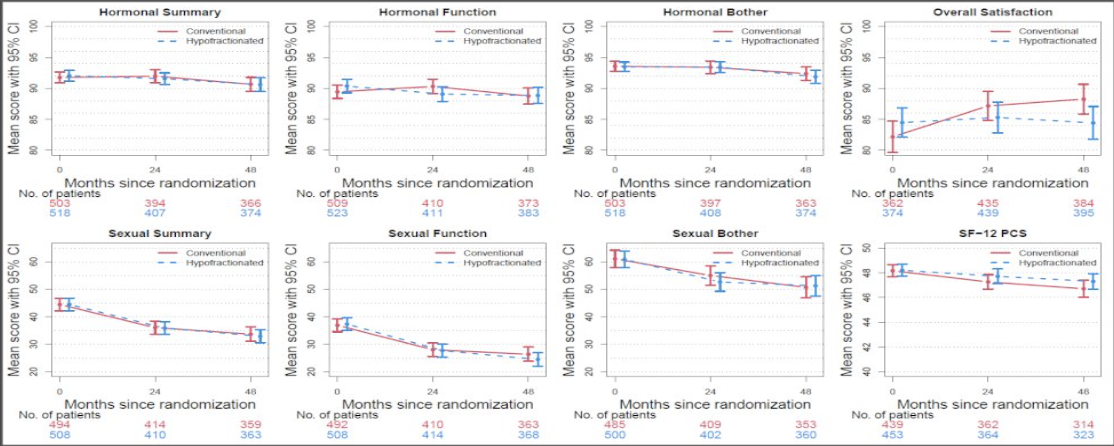
The SF-12 physical component score (PCS) and mental component score (MCS) were similar in both arms and remained stable throughout.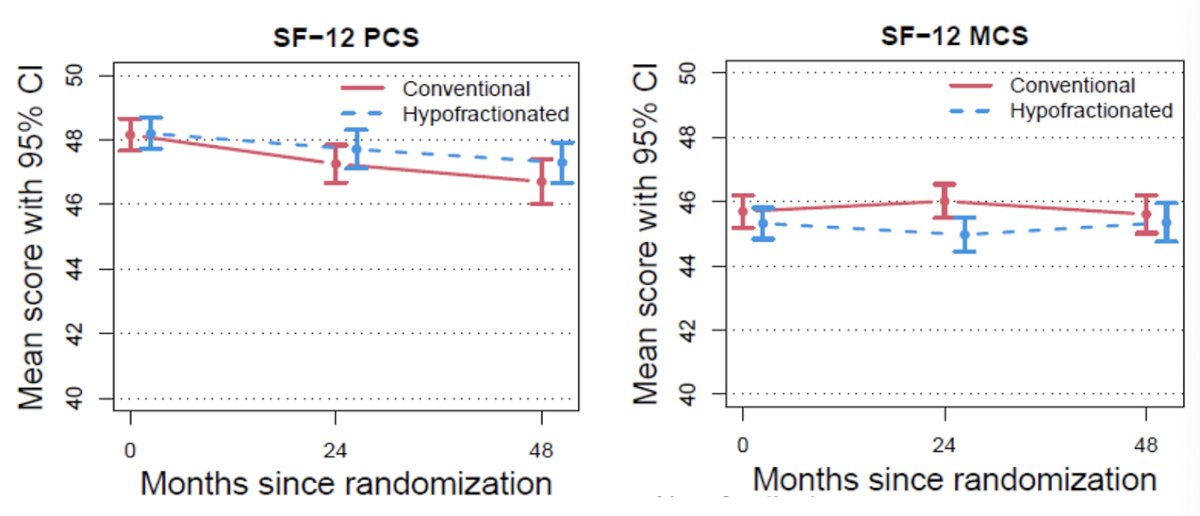
On multivariable analysis, the bowel summary and function scores were significantly worse in the
The overall satisfaction scores slightly favored the conventional fractionation treatment arm patients, as summarized below:
Dr. Sanmamed concluded as follows:
- Moderate hypofractionation (60 Gy in 20 Fr) was associated with similar health-related quality of life scores, compared with conventional fractionation (78 Gy in 39 fractions).
- These results are consistent with those of clinician-reported toxicity data.
- The proportion of patients reporting MID in bowel function at 48 months was significantly higher in the conventionally fractionated arm.
- Efficacy, toxicity, patient convenience, and now quality of life data all support the use of moderate hypofractionation as a standard of care option for the treatment of organ-confined prostate cancer.
Presented by: Noelia Sanmamed Salgado, MD, PhD, Radiation Oncologist, Hospital Clinico San Carlos, Madrid, Spain
Written by: Rashid Sayyid, MD, MSc – Robotic Urologic Oncology Fellow at The University of Southern California, @rksayyid on Twitter during the 2024 ASTRO Annual Congress held in Washington, DC between September 29th and October 2nd, 2024
References:- Hamdy FC, Donovan JL, Lane JA, et al. Fifteen-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N Engl J Med. 2023; 388(17):1547-58.
- Catton CN, Lukka H, Gu CS, et al. Randomized Trial of a Hypofractionated Radiation Regimen for the Treatment of Localized Prostate Cancer. J Clin Oncol. 2017; 35(17):1884-90.
- Lee WR, Dignam JJ, Amin MB, et al. Randomized Phase III Noninferiority Study Comparing Two Radiotherapy Fractionation Schedules in Patients With Low-Risk Prostate Cancer. J Clin Oncol. 2016; 34(20):2325-32.
- Dearnaley D, Syndikus I, Mossop H, et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. 2016; 17(8):1047-60.


