(UroToday.com) The 2024 American Society for Radiation Oncology (ASTRO) annual meeting held in Washington D.C., between September 29 and October 2 was host to the session EDU 16 - Management of Unfavorable Intermediate-Risk Prostate Cancer: Role of SBRT, Brachytherapy and Androgen Deprivation Therapy. Dr. Soumyajit Roy presented a Pooled Analysis of More than 13,000 Patients from 21 Randomized Controlled Trials, exploring the Natural History after Likely Cure vs. Recurrence after ProsTate RadiOtheRapy (RAPTOR).
In clinical practice, it is presumed that patients with localized prostate cancer are likely cured if there is no biochemical recurrence (BCR) within 5 years of receiving radiation therapy (RT) with curative intent. However, the natural history of the disease beyond this landmark period remains poorly understood and continues to evolve for patients both with and without BCR. Dr. Roy asked artificial intelligence (Google and ChatGPT) if a patient could be considered cured after 5 years of treatment with RT and no BCR. Both AI engines cautioned against the use of the word "cured" in this situation. Therefore, there is still significant ambiguity about what we believe happens after 5 years without BCR and what actually occurs.
This study was a pooled analysis of men enrolled in 21 randomized controlled trials with long-term follow-up to determine the incidence of subsequent cancer-specific events including distant metastasis (DM) and prostate cancer-specific mortality (PCSM) in patients with and without BCR within 5 years of RT completion. The investigators used individual patient data of patients who were treated with definitive RT with/without various durations of ADT based on the following 21 randomized trials:
- NRG/RTOG 0126, 9910, 9202, 9408, 9413, 9902
- EORTC 22961, 22991, 22863
- TROG RADAR, 9601
- MRC RT01, CHHIP
- GICOR/DART
- ICORG 9701
- PCS III, IV
- OTT 0101
- HYP062
- Fox Chase hypofx trial
The investigators estimated the cumulative incidence of distant metastasis using competing risk methods (Fine and Gray), considering any deaths as competing events. Similarly, the cumulative incidence of prostate cancer-specific mortality was estimated using competing risk methods, considering non-cancer-specific deaths as competing events. Additionally, multivariable competing risk regression models were applied to determine the adjusted association between BCR and post-BCR cancer-specific events. Lastly, the investigators tested for any heterogeneity in this association across different treatment strata.
A total of 13,468 patients across 21 trials were included in this meta-analysis. Approximately 30% (n=3,902) experienced a BCR event within 5 years. The median follow-up duration for these patients was 137 months (IQR 135 - 139). Among the 9,566 patients who did not experience BCR by 5 years, the median follow-up was 129 months (IQR 128 - 130).
The median age was 70 years, and the median PSA was 12.4 ng/mL. Most patients had clinical stage T1/T2 (72%) and Gleason grade group 2 or 3 (50%). The split between NCCN intermediate risk group (51%) and high-risk group (49%) was similar. The characteristics are shown in the table below: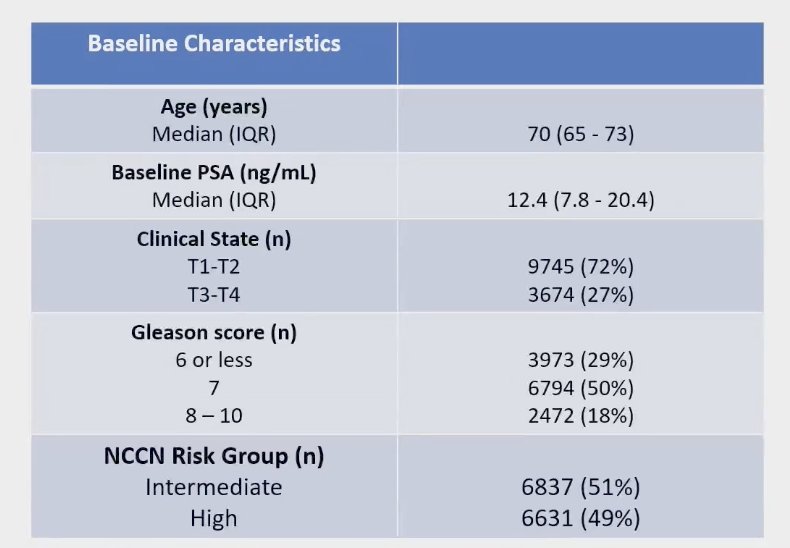
Distant metastases
In patients with BCR within 5 years, the incidence of distant metastases was 39%, compared to 3.3% in patients who did not experience BCR within 5 years. The cumulative incidence of distant metastases graphic is shown below: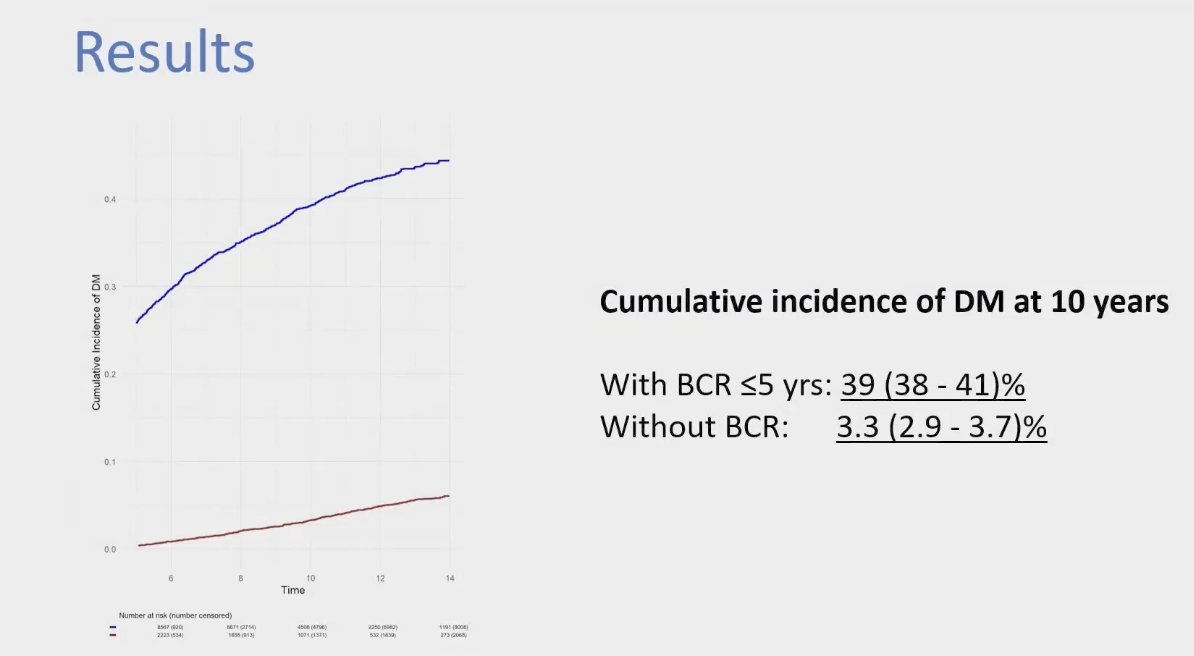
The cumulative incidence of PCSM at 10 years was 29% vs. 1.2% in patients who had BCR within 5 years compared to those without BCR, respectively.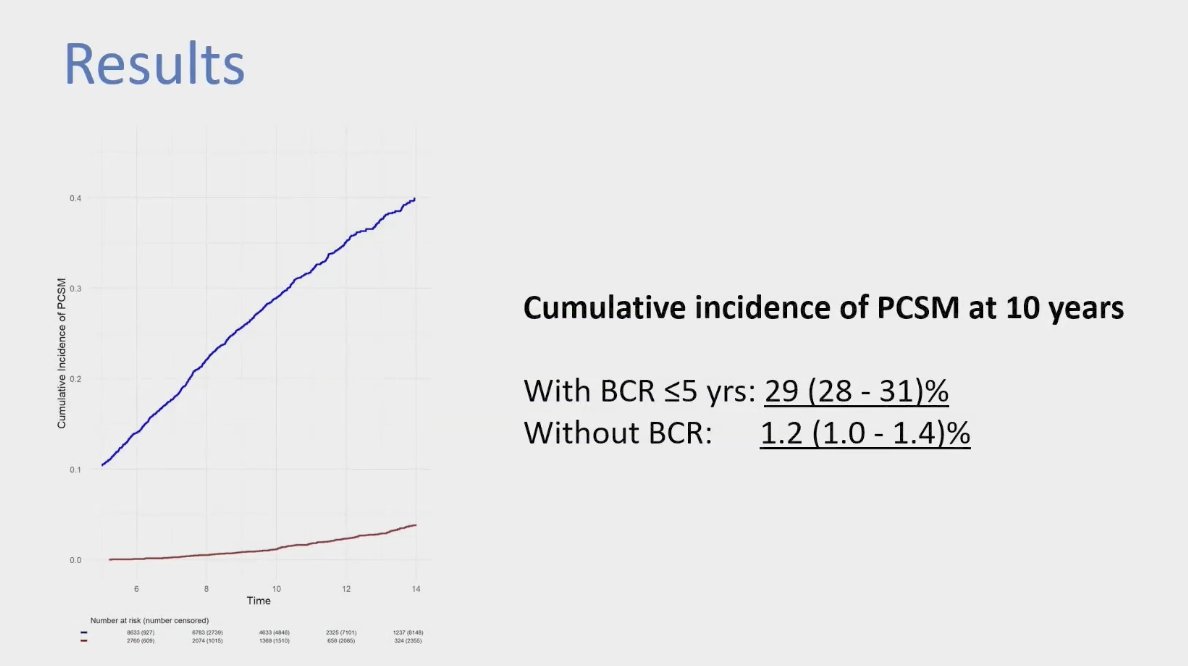
The investigators examined heterogeneity among the 21 studies included in this meta-analysis and found no statistically significant heterogeneity in the association of BCR within 5 years of RT with the post-BCR relative incidence of DM and PCSM across different treatment groups (p=0.24). The groups included in the analysis were dose-escalated RT alone, dose-escalated RT + long-term or short-term ADT, conventional dose RT alone, and conventional dose RT with short-term or long-term ADT.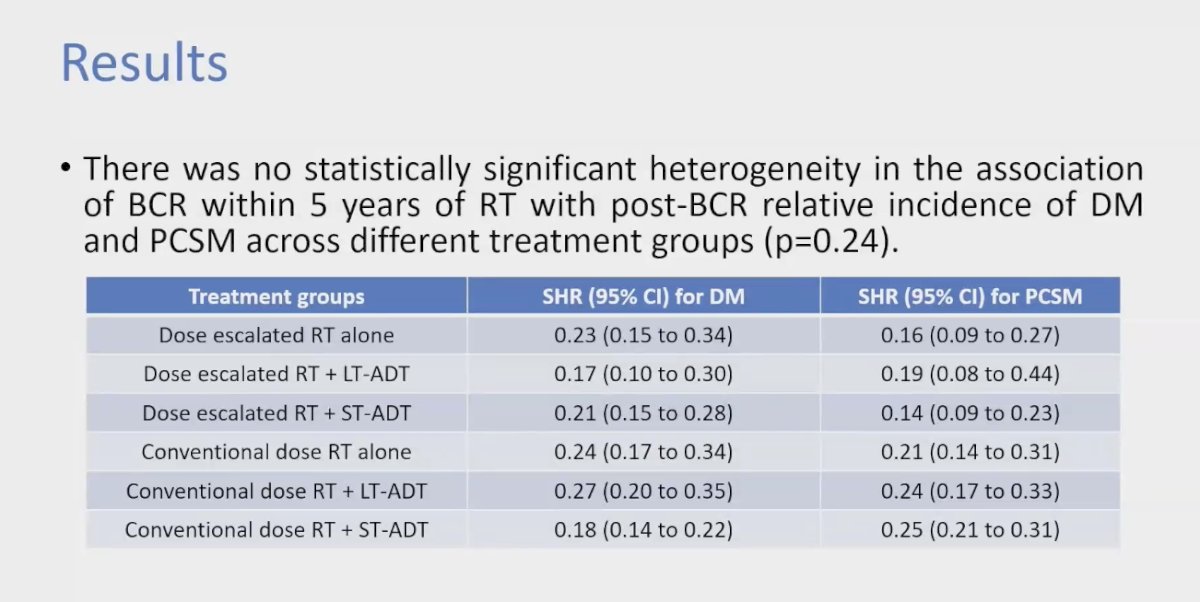
This pooled analysis was not without limitations. Dr. Roy acknowledged several constraints, including inter-trial variation in the definition of BCR, which the investigators plan to harmonize in the final manuscript. Additionally, there was a lack of information on grade grouping and stratification between favorable and unfavorable intermediate-risk groups, as Gleason reporting in Canada and Europe differed significantly from that in the U.S. There is also a possibility of misclassification bias regarding the cause of death. Furthermore, despite the median follow-up being 12 years, this duration may still be insufficient to adequately assess PCSM and DM in patients with localized prostate cancer treated with curative intent RT.
Dr. Roy wrapped up his presentation with the following conclusions:
- BCR within 5 years of RT is prognostic for distant metastasis and cancer-specific mortality.
- Every 2 in 5 patients with BCR within 5 years can develop distant metastasis within the next 5 years and every 1 out of 3 patients with BCR can die from their prostate cancer in the next 5 years.
- In contrast, patients without BCR by 5-years of RT can be "safely" considered to be cured given the limited event rates in this group.
- BCR despite being prognostic for MFS or PCSM is not a surrogate for OS.
Presented by: Soumyajit Roy, MS, MBBS, PGY5 Department of Radiation Oncology at Rush University Medical Center, Chicago, IL, United States of America
Written by: Julian Chavarriaga, MD – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Society for Radiation Oncology (ASTRO) annual meeting held in Washington D.C., between the 29th of September and the 2nd of October.


