(UroToday.com) The 2024 American Society for Radiation Oncology (ASTRO) Annual Meeting held in Washington, DC between September 29th and October 2nd, 2024, was host to a prostate cancer treatment intensification session. Dr. Comron Hassanzadeh presented the long-term results of a phase III randomized trial comparing hypofractionated, dose-escalated radiotherapy to conventionally fractionated radiotherapy for clinically localized prostate cancer.
Hypofractionated and conventionally fractionated prostate radiotherapy have been evaluated in both non-inferiority and superiority trials with variable biologic doses. Summarized below are the 4 non-inferiority trials published in this space, to date: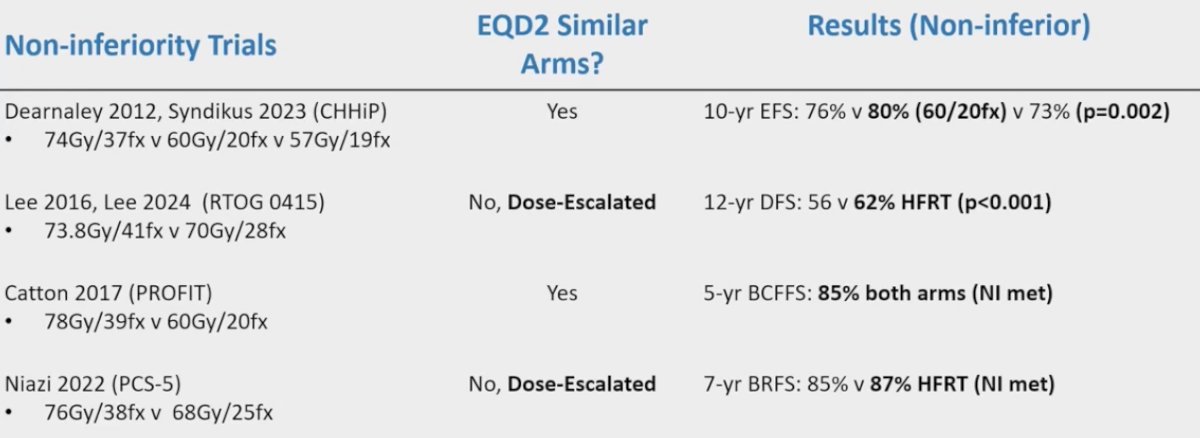
While the non-inferiority of hypofractionation has been proven, Dr. Hassanzadeh noted that the superiority of this modality remains uncertain.
Notably, there has been an increased adoption of hypofractionated, including ultra-hypofractionated (i.e., SBRT) radiotherapy, especially following the COVID-19 pandemic. Only ~30% of patients nationwide receive conventional fractionation for intermediate-risk prostate cancer.1
The study objective was to evaluate whether dose-escalated, hypofractionation (HIMRT) was associated with superior cancer control outcomes compared to conventional radiotherapy (CIMRT) for men with localized prostate cancer.
The study design is summarized below. This trial included prostate adenocarcinoma patients with cT1b-3b disease, PSA ≤20 ng/ml, Gleason Score <10, and no evidence of nodal or bone metastases. Patients underwent stratified randomization 1:1 to either CIMRT or dose-escalated HIMRT, between January 2001 and January 2010.
The treatment regimens were as below:
The primary study endpoint was biochemical failure, defined as PSA nadir + 2 (Phoenix criteria) and/or the need for initiation of salvage therapy. Secondary endpoints included:
- Patient-reported acute/late GI and GU toxicity
- Physician-reported acute/late GI and GU toxicity
- Prostate cancer-specific survival
- Overall survival
This was a superiority trial, with 91% power to detect a 20% difference in freedom from failure at 5 years, with an estimated 39 events required.
The treatment arms were well-balanced for patient characteristics. ~75% of patients in this trial were considered intermediate-risk, and ~25% received neoadjuvant ADT.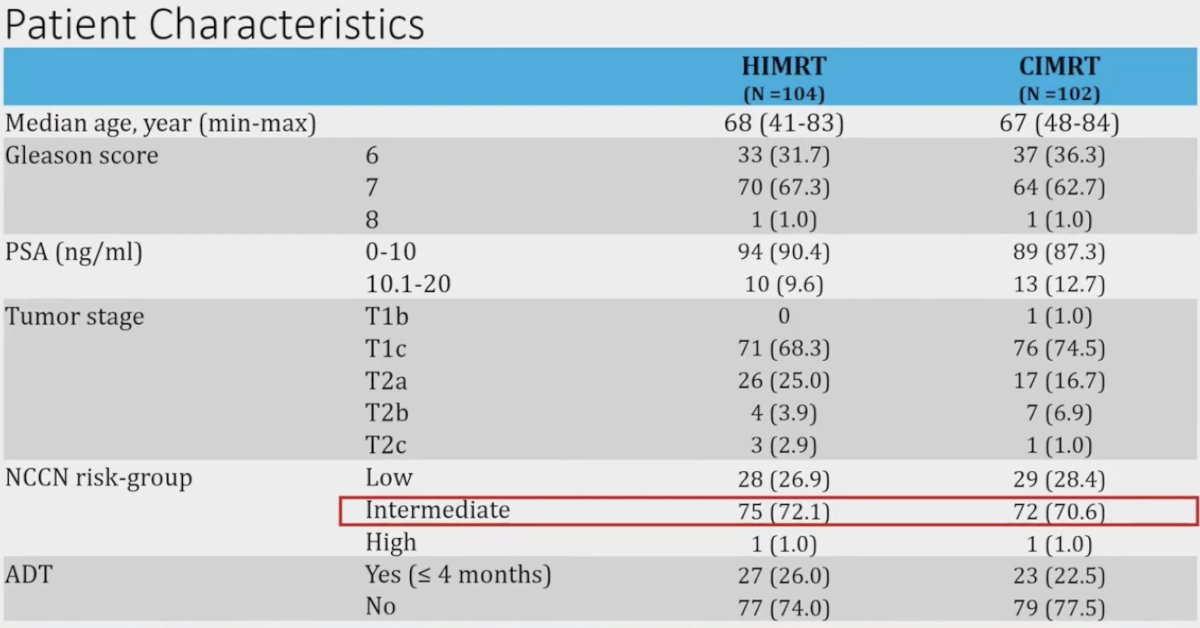
While not reaching statistical significance, there was a considerable improvement in treatment failure rates with HIMRT, with 10-year rates of 11% versus 21% (p=0.077).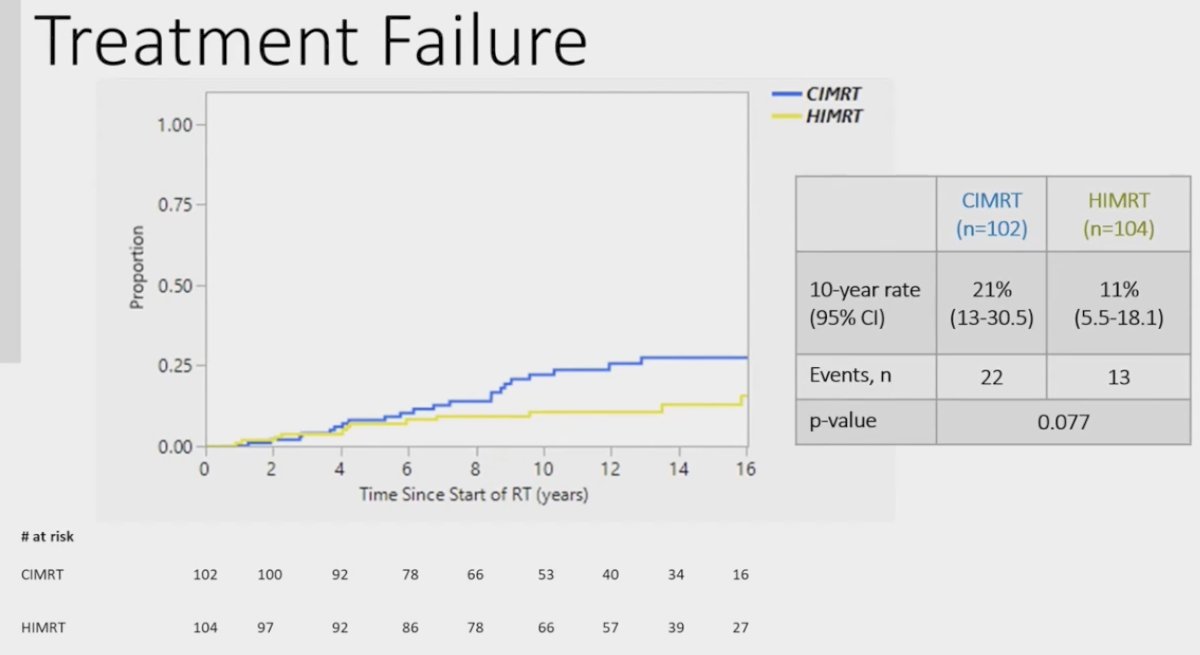
This trend held true and reached statistical significance when analysis was limited to the population that did not receive ADT:
Distant metastases were rare event in this predominantly intermediate-risk cohort, with only 1 and 4 events in the CIMRT and HIMRT cohorts, respectively.
With regards to late toxicity, the 10-year rate of GI grade ≥2 events was higher in the HIMRT group (13% versus 5%, p=0.08). There were no differences in the 10-year rates of GU grade ≥2 toxicity.
Dr. Hassanzadeh concluded as follows:
- HIMRT has become standard of care for intermediate-risk prostate cancer
- There were no peaks in late toxicity and sustained efficacy of HIMRT on long-term follow-up
- Better for patients who had not received neoadjuvant ADT?
- What is the ideal dose/fractionation regimen for prostate radiotherapy?
- 60 Gy/20 fractions versus 70 Gu/28 fractions versus SBRT?
- Appropriate patient selection is key here.
- 60 Gy/20 fractions versus 70 Gu/28 fractions versus SBRT?
Presented by: Comron Hassanzadeh, MD, MPH, Assistant Professor, Department of Radiation Oncology, Division of Radiation Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX
Written by: Rashid Sayyid, MD, MSc – Robotic Urologic Oncology Fellow at The University of Southern California, @rksayyid on Twitter during the 2024 ASTRO Annual Congress held in Washington, DC between September 29th and October 2nd, 2024
References:

