(UroToday.com) The 2024 ASTRO annual meeting included a session on novel prognostic tools in prostate cancer, featuring a presentation by Dr. Anna Dornisch discussing P-CARE, a model to stratify risk of any, metastatic and fatal prostate cancer. Prostate cancer screening is controversial and there are many guideline-based recommendations: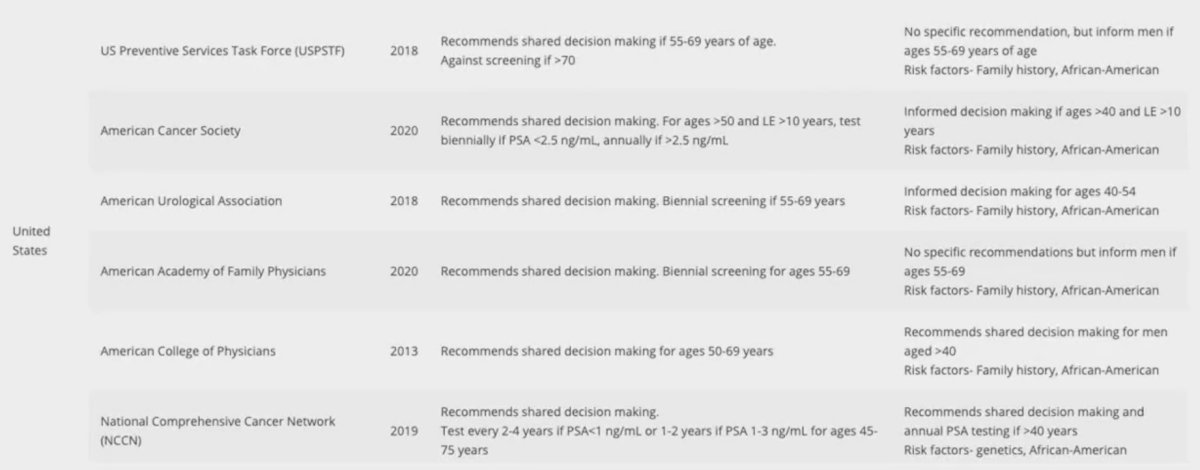
Common tenets of prostate cancer screening guidelines include shared decision-making and individual risk assessment. However, subjective risk assessment based on family history and race is neither accurate nor consistent. A polygenic hazard score based on 290 genomic variants (PHS290; calculated from a single saliva sample) is strongly associated with age at diagnosis of aggressive prostate cancer in large datasets, including the racially and ethnically diverse Million Veteran Program:1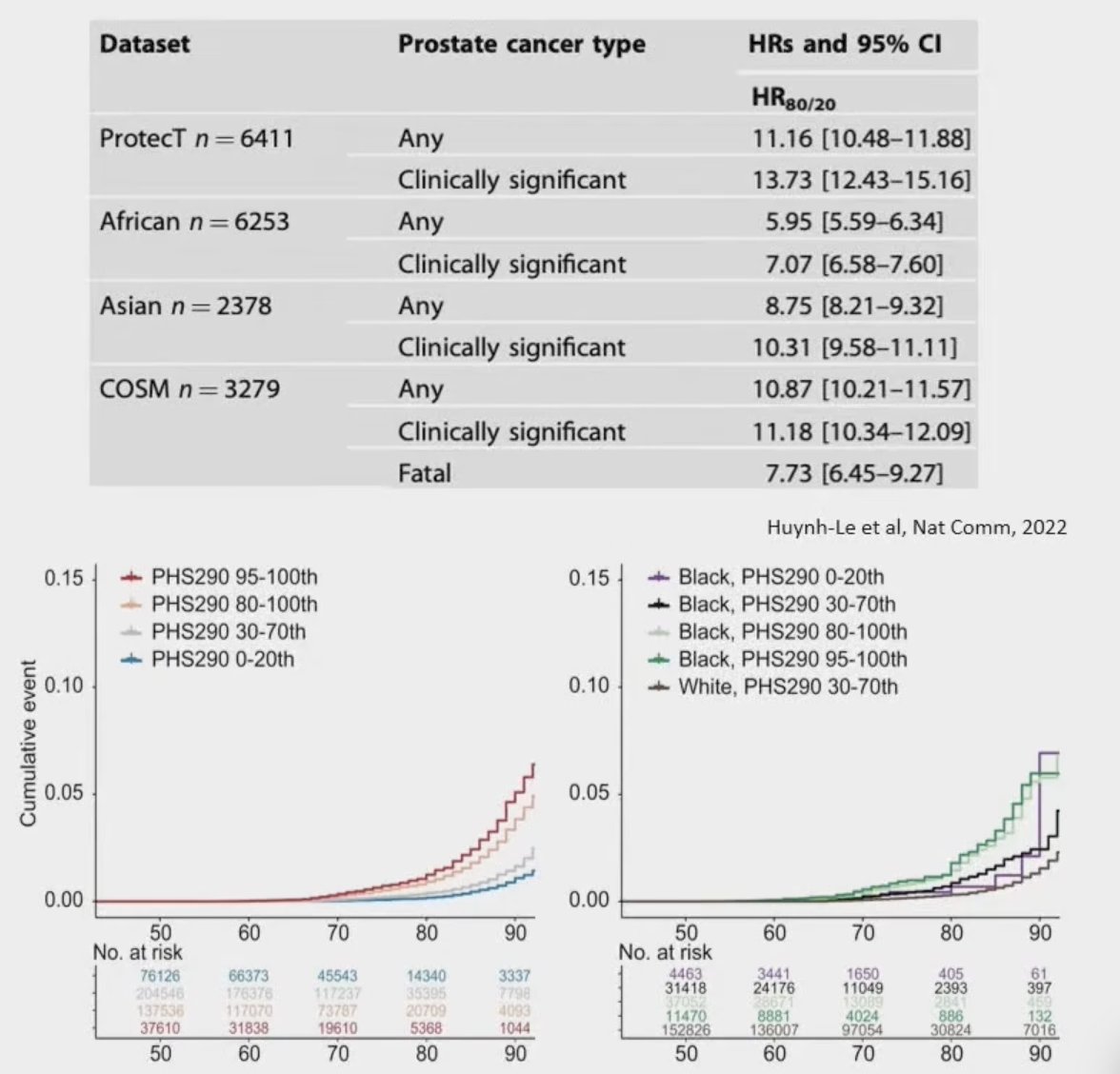
Moreover, PHS290, ancestry, and family history are each independently associated with lifetime risk of metastatic prostate cancer. At ASTRO 2024, Dr. Dornish and colleagues presented data assessing development and validation of a new integrated model for use in the primary care setting, called Prostate Cancer integrated Risk Evaluation (P-CARE).
Candidate genetic variants in the literature with reported association with prostate cancer, aggressive prostate cancer, benign prostatic hyperplasia, or benign PSA elevation were considered for inclusion in the new PHS model. The investigators used genetic and phenotypic data from a diverse, population-based cohort (Million Veteran Program, n = 585,418). They then fit a LASSO-regularized PHS model using the age at diagnosis of prostate cancer as the time to event, and all the candidate genetic variants as predictors while covarying the first 5 principal components of genetic ancestry. Next, they combined the new PHS with family history and ancestry to create an integrated risk score, P-CARE, again using age at diagnosis of prostate cancer as time to event. Finally, they estimated the hazard ratio performance of the new PHS model and P-CARE using 10 iterations of a 10-fold cross-validation. This study found 707 unique candidate variants, of which 601 were ultimately included in the updated polygenic score (PHS601). P-CARE combined PHS601, family history, and agnostic genetic ancestry. Risk stratification with PHS601 for the highest 20% risk (vs the lowest 80% risk) had a hazard ratio for metastatic prostate cancer of 6.69 (95% CI 5.70-7.62):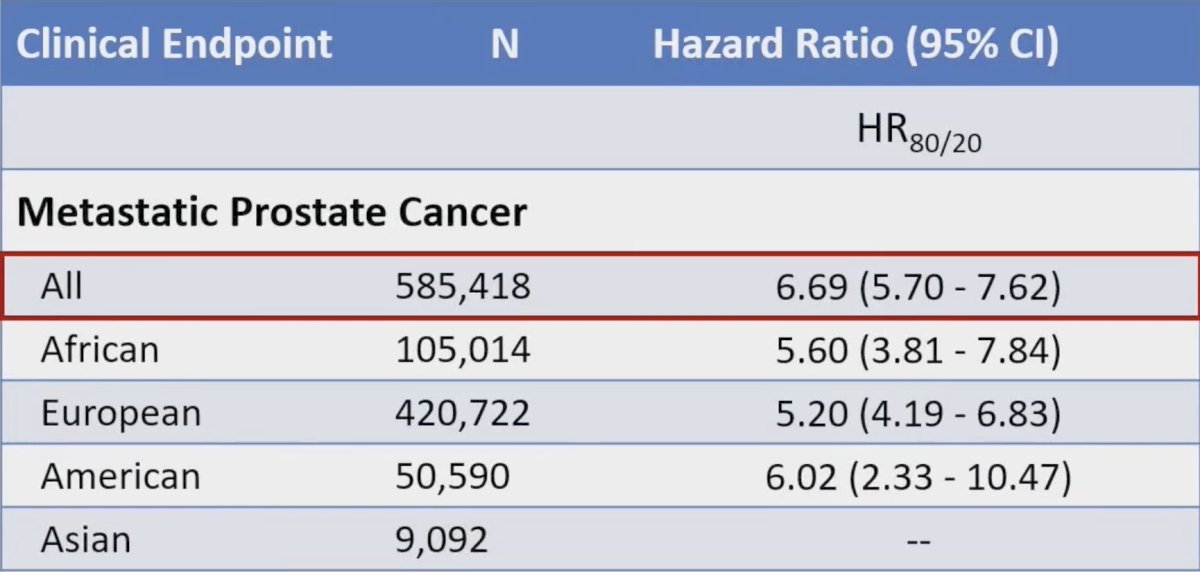
Risk stratification with P-CARE for the highest 20% risk (vs the lowest 80% risk) had a hazard for metastatic prostate cancer of 6.50 (95% CI 5.50-7.38):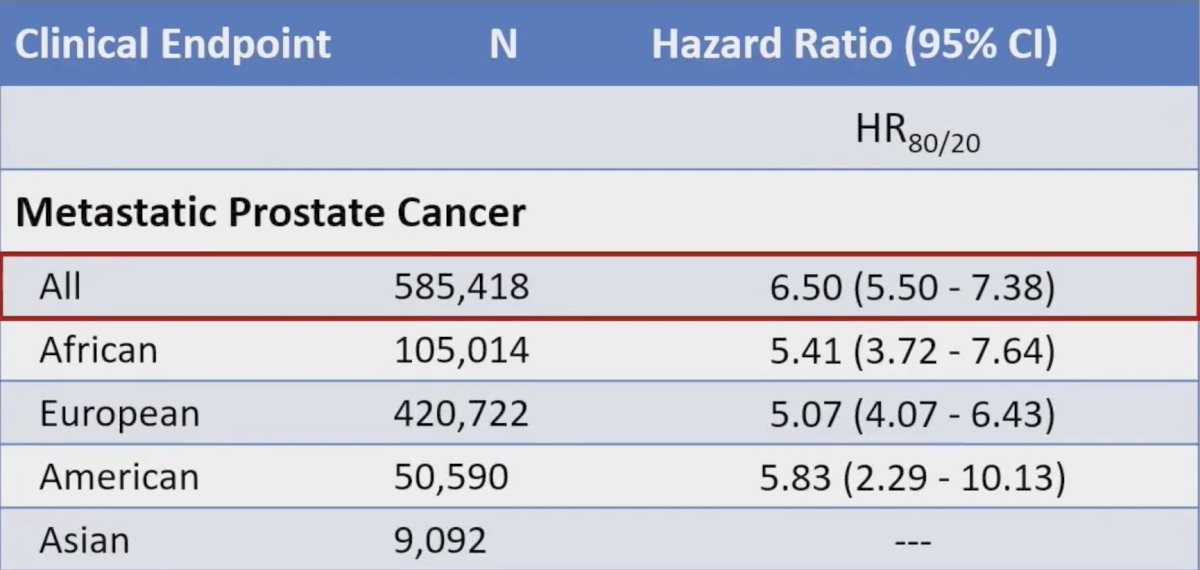
The following shows the cumulative incidence curves, as well as highlighting that those men with high risk, have a 21.2% risk of developing prostate cancer by age 70: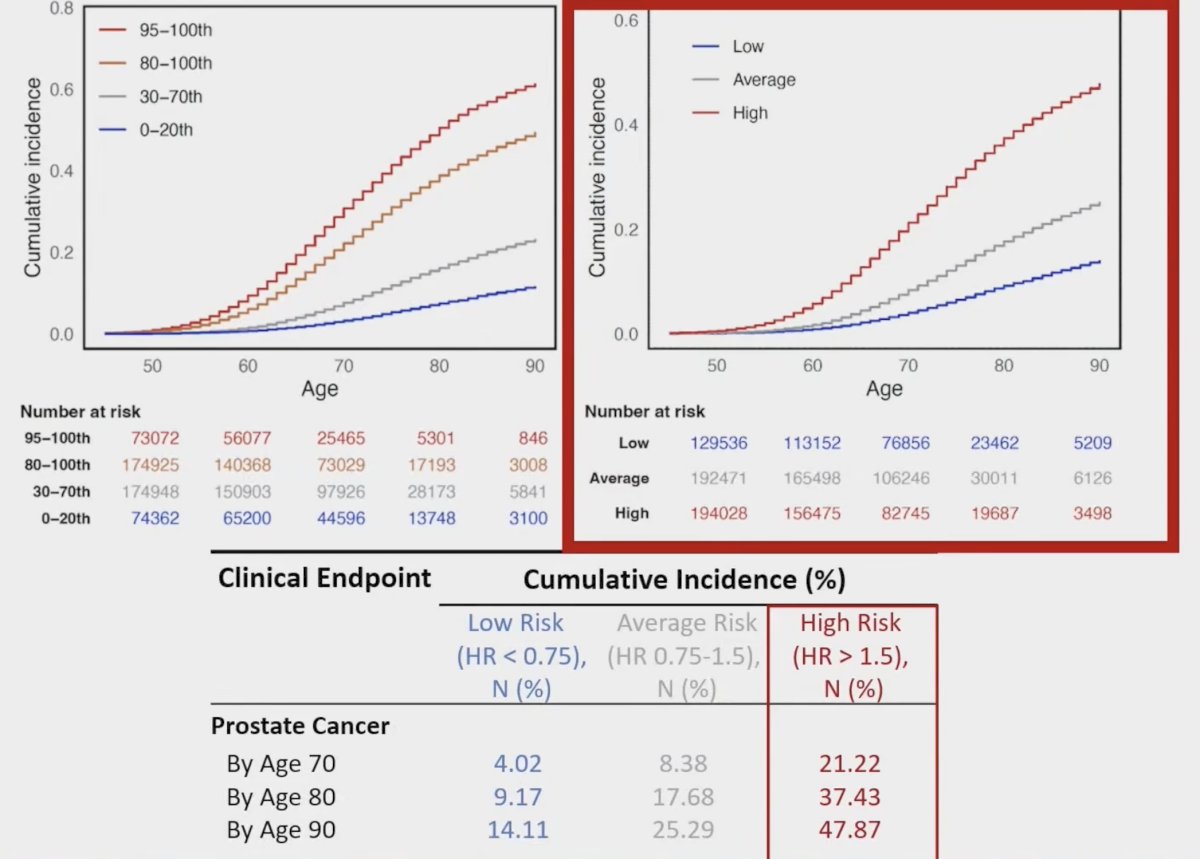
Furthermore, the following shows the cumulative incidence curves, as well as highlighting that those men with high risk, have a 21.2% risk of developing metastatic prostate cancer by age 70: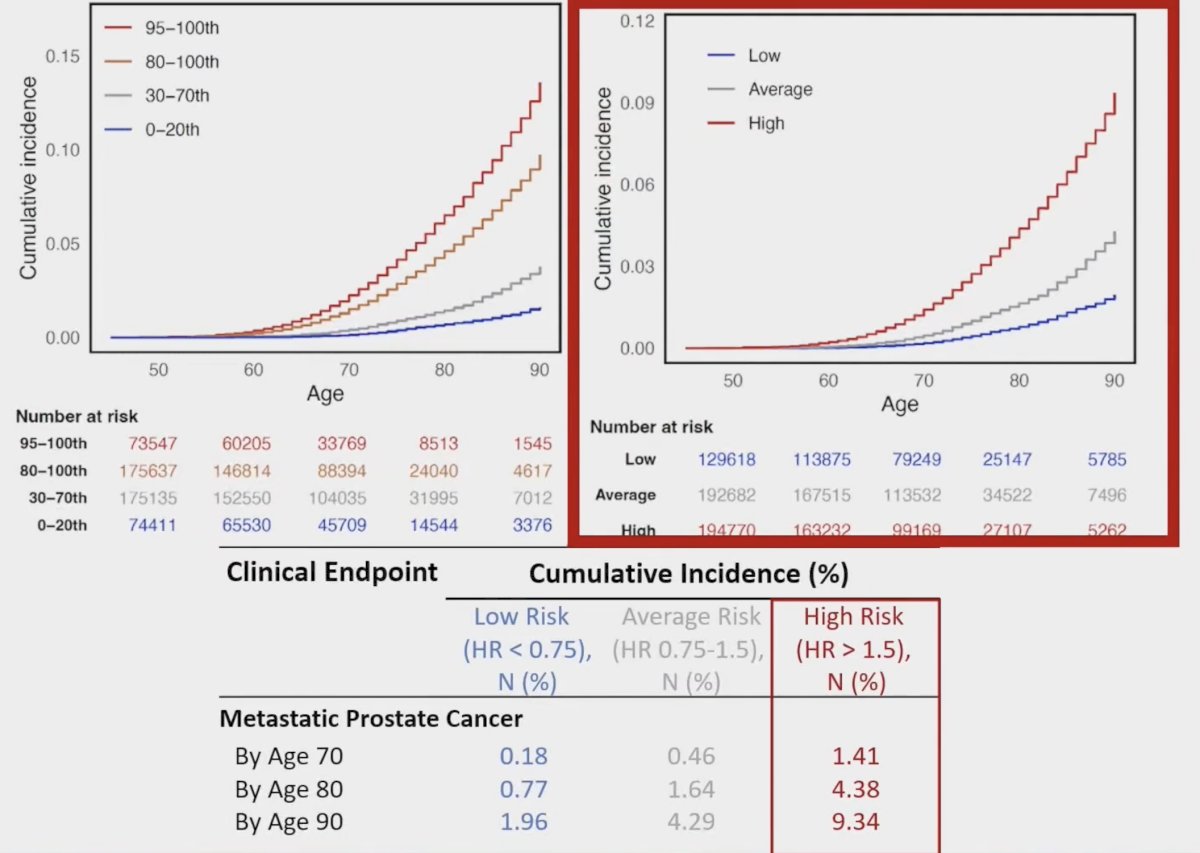
Dr. Dornisch concluded his presentation discussing P-CARE, a model to stratify risk of any, metastatic and fatal prostate cancer with the following take-home points:
- P-CARE provides a single, objective score that can be used in the primary care setting to stratify patients for risk of meaningful prostate cancer
- The investigators will use P-CARE in a nationwide randomized clinical trial to evaluate precision prostate cancer screening in the VA healthcare system (ProGRESS: The Prostate Cancer, Genetic Risk, and Equitable Screening Study NCT05926102)
Presented by: Anna Dornisch, MD, Radiation Oncologist, UC San Diego, La Jolla, CA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Society for Radiation Oncology (ASTRO) Annual Meeting, Washington, DC, Sun, Sept 29 – Wed, Oct 2, 2024.
Reference:


