- Biologic barriers – surgery, chemotherapy, radiotherapy, immunotherapy, and metabolic manipulation.
- Best practice barriers
- Social Barriers – access to treatment, distance, and complexity of postoperative care

Figure 1 – Cancer-specific survival association to the stage of bladder cancer after radical cystectomy, Shariot et al J. Urol 2006, Penn Urology
Unfortunately, when looking at The Surveillance, Epidemiology, and Ends Results (SEER) US-population based data, only 21% of patients with MIBC underwent radical cystectomy and diversion as their method of care.1 It was shown that rising age, increasing comorbidities, and increasing travel distance negatively impacted the choice of treatment. As expected, the overall 5-year survival was superior for patients who underwent radical cystectomy vs. radiotherapy/chemotherapy, and surveillance (42.2% vs. 20.7% vs. 14.5%, respectively). Radical cystectomy is apparently a critically underused treatment modality of MIBC.
Neoadjuvant chemotherapy has been proven to give a 5% overall survival absolute benefit over 5 years. The use of neoadjuvant chemotherapy has been increasing through the years, as shown in the national cancer database (NCDB) from less than 10% in 2006 to more than 30% in 2016.2
Increased hospital volume and surgeon experience positively affect the overall mortality rate of radical cystectomy. When surgery is performed, it should be performed optimally, with negative surgical margins, and a large node yield from an extended pelvic lymph node dissection.
There have been significant advancements in the understanding of the genetic pathogenesis of MIBC, with more understanding of the new and various divisions of MIBC to molecular subtypes. These subtypes allow us to predict which MIBC will respond better to neoadjuvant chemotherapy, and which will have better survival rates. Figure 2 is a diagram summarizing sensitivity to chemotherapy and immunotherapy of the various molecular subtypes.
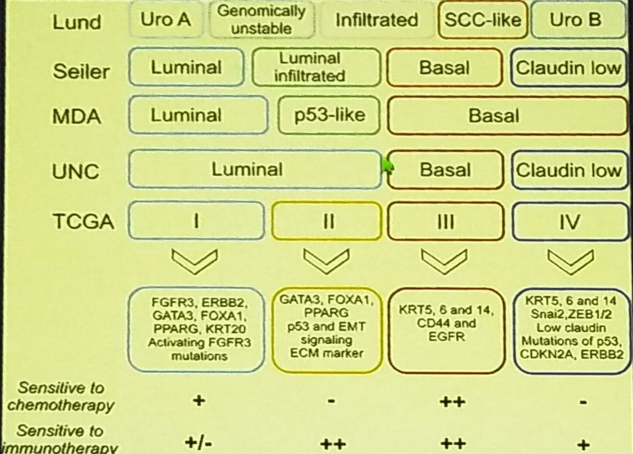
Figure 2 – Sensitivity to chemotherapy and immunotherapy according to the various molecular subtypes of muscle-invasive bladder cancer, Knowles Nat Com 2018
There are new and classic targets in the treatment of MIBC. These include cell cycle regulators (TP53, RBI), signal transduction pathways, epigenetic changes, and other involved genetic mutations. Immunotherapy has been introduced as a major new player, but with all the excitement around these new drugs, it is important to note that their added benefit is in only 15-20% of patients, with only several months of added overall survival benefit.
In summary, MIBC therapy should be maximized with the implementation of all known improvements of patient outcomes. These include optimizing radical cystectomy – making sure it reaches all patients it needs to be reached too, and that the quality of the procedure is maximized through centralization of care. This means extended pelvic lymph node dissection, and negative surgical margins. Precision medicine will continue to evolve and immunotherapy will need to be expanded further. Newer targets of therapy should be introduced, including metabolic manipulation.
Presented by: S. Bruce Malkowicz, MD, Professor, Division of Urology, Department Of Surgery, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA
References:
1. Gore and Litwin et al. JNCI 2010
2. Hanan et al. CUA 2016
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, @GoldbergHanan at the 70th Northeastern Section of the American Urological Association (NSAUA) - October 11-13, 2018 - Fairmont Royal York Toronto, ON Canada


